This is the multi-page printable view of this section. Click here to print.
Documentation
- 1: Overview
- 2: Basic Science
- 2.1: What are steroid hormones?
- 2.2: Sex Hormones: how do they work?
- 2.3: The different estrogens, androgens and progestogens, and their binding affinity
- 2.4: The self-regulation mechanism, and how to use it in our benefits
- 2.5: Growth hormones
- 2.6: DHEA and intracrinology
- 3: Feminizing HRT
- 3.1: The different methods
- 3.2: SHBG: What is it, and why it can matter
- 3.3: Estrogens
- 3.3.1: Transdermal gel and patches
- 3.3.2: Oral
- 3.3.3: Injections
- 3.3.4: Pellets
- 3.3.5: Sources on the risks of thrombosis
- 3.4: Androgen blockers and progestogens
- 3.4.1: Androgen receptor blockers: Spironolactone and Bicalutamide
- 3.4.2: Inhibitors of 5a-reductase: Finasteride and Dutasteride
- 3.4.3: GnRH agonists and antagonists (“Puberty blockers”)
- 3.4.4: Synthetic progestogens (Androcur...)
- 3.5: Progesterone
- 3.6: Maintaining erections and healthy penile tissue: topical testosterone
- 3.7: That was a lot... So, what should I take?
- 4: Masculinizing HRT
- 5: Injection guide
- 6: Blood tests, other screenings and neovaginal health
- 7: Gender affirming surgeries
- 7.1: MtF/MtX Surgeries
- 7.2: FtM/FtX surgeries
- 8: Reference
- 8.1: Parameter Reference
- 9: Contribution Guidelines
1 - Overview
You are here in the documentation section, where we provide detailed ressources and information on most medical aspects of gender transitions.
All information is sourced from scientific literature. We write a warning in case an info is only experimental or hypothetical.
We are a small team of volunteer working on our free time; for this reason, source references are not present everywhere yet. We will update sources regularly and as soon as possible.
If you are not acquainted with the general science behind hormone therapy, we advise you to start with the “Basic science” folder, and read it in the proposed order, since the information builds up on each previous page.
2 - Basic Science
The six pages of this section are aimed at giving you general information on hormones - and more specifically sex hormones - and other biological functions involved in transgender Hormone Replacement Therapy (HRT). If you don’t know much about this, we recommend reading them in the proposed order, since they’ll build on each other.
2.1 - What are steroid hormones?
Sex hormones such as estrogens, androgens and progestogens, are all “steroid hormones”. This page describes the role of hormones, and the subgroup of steroid hormones.
First of all, what are hormones? Hormones are chemical substances produced by the body, and functioning as a messenger between organs. There is usually an organ that produces and an organ that receives. You can think of hormones as the wireless counterpart of the nervous system. It connects parts of the body remotely, to give them various orders; and it is much slower than the wired nervous system. Some common and known hormones that act as neurotransmitters are dopamine, serotonin, oxytocin, melatonin… Closer to our topics, we find the GnRH (Gonadotropin Releasing Hormone), FSH (Follicle Stimulating Hormone) and LH (Luteinizing hormone). Those last three, as we’ll see, play an important role in controlling sex hormones, and we’ll see what we can do with that.
So, the hormones that interest us here, the “sex hormones” - estrogens, androgens, and progestogens - are steroids that act as hormones. That’s why we call them steroid hormones. And those three groups - androgens, estrogens, and progestogens - are only three among five subgroups of steroid hormones; the two other being glucocorticoids (like cortisone and cortisol - the so-called stress hormone), and mineralocorticoids. We don’t need to know about those two here.
So what are steroids, and what do they have to do with “steroids” used by some bodybuilders and intense sportspeople (you know, -“this guy is buying steroids online, he wants to grow bigger and bigger!) ? Well, the products that these sportspeople use are part of the same group of molecules called steroids - and they are grouped together because of their particular molecular composition and organization, and the way they interact with their target cells. Steroids used in sports are a subgroup of steroid hormones called anabolic steroids, and it includes “natural” androgens like testosterone, but many other synthetic androgens. Anabolic steroids are all androgenic - various molecules similar to testosterone, and activating the androgen receptors -, but we chose here to speak of anabolic steroids to designate both “natural” (biosynthesized, naturally present in the body) and synthetic androgenic hormones (including the one used and abused in sport); and androgens to designate only the bioidentical molecules produced by the body (mainly testosterone and DHT).
But, yes, if you get estrogen treatment to grow boobs, then you can say that technically, you’re taking steroids. Not anabolic, but steroid still.
But let’s keep it simple and call them hormones, because they act just like hormones.
2.2 - Sex Hormones: how do they work?
The hormones that interests us for trans HRT are sex hormones. Those are an informal subgroup of steroid hormones. We’ll discuss here how hormones have effects on our bodies, and learn about the importance of “receptors”.
And first, what are they? As we said before, sex hormones is a group that covers 3 subgroups of steroid hormones: androgens (among which the famous testosterone), estrogens (estradiol will be our main friend for feminizing HRT), and progestogens (progesterone is the main naturally occuring one). That’s why they are sometimes called sex steroids, but also gonadal steroids, since they are mostly produced in our gonads: testes and ovaries.
It is common to picture the mode of actions of hormones as the key and keyhole image. The hormones are keys that circulate in the body until they reach a cell with the right keyhole. We call those keyholes receptors. Estrogens are all the keys that can only open estrogenic keyholes (receptors) - be it synthetic or natural estrogens, and the same goes for androgens.
We all have those different receptors: it is not because you were assigned male at birth and produce mostly testosterone that your cells won’t have estrogen receptors. If it were the case, HRT for trans people would not work at all. There can be, however, differences between people, moments of life, and hormone balance exposure, in terms of the repartition and sensitivity of those receptors in the body cells.
If the binding happens (the key gets into the hole), then the cell is given the order to express a certain aspect of itself coded in DNA. For example, when an estrogen hits and opens the receptor of skin cells, those cells get the message to produce less sebum, which leads to less greasy skin - in the limits given by the DNA. In other words, sex hormones will only “unlock” and express what is already coded in DNA, which cannot be changed by any medication. This explains the differences in development observed between people with the same profile and the same hormone levels.
In short, we call estrogens all hormones that fit in the estrogen receptors, androgens all those that fit in the androgens receptors, and the same goes for progestogens. And this means that there is not just one estrogen, androgen, and progestogen. Let’s have a look now at these different kinds of each sex hormone, and why it matters to know about them.
2.3 - The different estrogens, androgens and progestogens, and their binding affinity
When we speak of estrogens, we don’t refer to only one hormone. Estrogens, as well of androgens and progestegens are three groups, each covering similar yet different hormones. Knowing about those differences is important in many ways.
Let’s speak first of binding affinity. Binding affinity designates the ability and “ease” with which one hormone will bind to its receptor. If we use the key and keyhole metaphor, you can imagine that several keys can open the same lock, but some will enter and turn with much difficulty, when others will do it quite smoothly. This is binding affinity: it is high when the key gets in without effort, and opens efficiently, and it is low when the key can open the lock, but not without effort. The different kinds of each sex hormone come with different binding affinity, which is why we will prefer some over others for efficient feminization/masculinization.
If we take a look at estrogen first, we can count four of them present in the body (at least the main ones) in differents amount: Estrone (E1), Estradiol (E2), Estriol (E3) and Estetrol (E4). But really, keep in mind only estradiol (E2), and to a lesser extent estrone (E1). Estradiol is the main active estrogen in our bodies, and it has a much higher binding affinity than estrone, so that is the one we will use for feminizing HRT. There are also a number of synthetic estrogens, developed by pharmaceutical laboratories in particular for the use in birth control pills: a common one is Ethinylestradiol (EE). As a synthetic derivative of estradiol, EE also comes with more (and more frequent) side effects. This is why it is not recommended to use birth control pills for feminizing HRT.
Note
Actually, research has shown that the common side effects of estrogen therapy that trans women are usually warned about by practitioners - and used as a reason to keep them at low doses of estrogens - such as blood clots, are mostly associated to synthetic estrogens (like EE), and to a much lesser extent to bioidentical estradiol. If you don’t have predispositions to thrombosis (comorbidities and/or genetic background), taking bio-identical estradiol - even in relatively high doses - should not be a big problem. Estrone (E1), even though bioidentical, is also associated with more frequent side effects, which is why you want to avoid oral administration of estradiol pills: indeed, most of the estradiol (E2) it contains is converted into Estrone (E1) by the liver first pass. A good way to avoid the hepatic first pass while taking oral pills is the “sublingual method”, which consists in letting the pill melt completely under the tongue. This way, estradiol is directly absorbed by the mucous membrane of the mouth, and reaches the bloodstream without passing through the liver first pass.
Let’s now have a look at androgens. We mostly know of testosterone, and it is indeed the most present androgen naturally produced by the body. However, the body is also able to convert testosterone into a much more potent form in terms of masculinizing effects: DHT (dihydrotestosterone). This conversion is made with the help of an enzyme called 5a-reductase - which is good to know since a number of antiandrogens medication (Finasteride and Dutasteride) prescribed to transfeminine people consists in inhibiting this enzyme and by doing so preventing the conversion of testosterone into its more potent form, DHT. And there are finally all the synthetic androgens that we put before in the category of anabolic steroids.
The same goes for progestogens: the main - naturally occurring - one is progesterone; but pharmaceutical labs have also created a vast amount of synthetic progestogens, lots of them - once again - for the use in birth control medication. The well known cyproterone acetate (Androcur) is one of them; and even though it is a progestogen that activates the progestogens receptors, its action (and side effects) is far from being the same as bioidentical progesterone. Another progestogen commonly found in birth control pills is Levonorgestrel.
2.4 - The self-regulation mechanism, and how to use it in our benefits
The negative feedback mechanism is a normal and “natural” biological function of the endocrine system that regulates the production of sex hormones, so that we don’t end up with too much or too little. Knowing about this mechanism is key to understanding many methods of HRT, and the way some medications work.
If the body naturally and continuously produces sex hormones, why don’t we end up with too much of them? Well, obviously because the body is smart and able to self-regulate the production. And understanding the way it does that can help us understand and choose better the ways of our medical transitions (at least for transfeminine people).
The production of sex hormones is the final step of a chain of signals and reactions that starts in the brain. A part of the brain (the hypothalamus) releases in a pulsatile way (i.e. in a regular temporal pattern) a hormone called GnRH (Gonadotropin releasing hormone). GnRH is received by a gland in the lower part of the brain - the pituitary gland (or hypophysis), which, in response, releases two hormones called gonadotropins: FSH (Follicle Stimulating Hormone) and LH (Luteinizing hormone). Those two will go down to the gonads (ovaries and testes) which, in response, will produce testosterone (for the testes), and estradiol and progesterone (for the ovaries).
This sex hormone production will continue, and the levels of estradiol/progesterone/testosterone will rise, and circulate in the body. They will be received by the brain, and after reaching a threshold, eventually send the signal to both hypothalamus and hypophysis to stop the production of both GnRH, and FSH/LH. In other words, when the sex hormones reach a level that the body judges to be correct, they turn into a messenger ordering to stop their own production. This part of the circle is what we call negative feedback.
It should be noted that this mechanism is a bit more complex for AFAB people with a full reproductive system, as the regulation of hormones must allow for the cycle to work with the different phases (stimulation, ovulation, menstruation…). We will not detail this system here as this is not a website about reproductive health.
Now, what does this mean for us? It means that we have a way to control the production of our sex hormones - or at least to stop them.
- On the one hand, the brain will respond indifferently to all androgens, estrogens and progestogens to activate the negative feedback. For the brain, they are all read as sex hormones.
- On the other hand, the gonads can produce only one type of hormone, the one type whose production will be stopped by the negative feedback mechanism. That means that by adding enough of any sex hormone in the bloodstream from the outside (this is called exogenous - from an outside source - as opposed to endogenous - body made), and even if it is not the hormone that your body produces naturally, you can stop the production of the only hormone your body can produce.
So, in the case of feminizing HRT, we add exogenous estradiol; if the levels are high enough, the brain will receive the signal “ok, enough sex hormones” and send the signal to the gonads: “stop the production”. If you’re AMAB, with testes, the only thing your body can do is to stop the production of testosterone. If you keep this level, you end up with the ideal hormonal balance for feminization. Your estradiol will be medium-high to high, your testosterone will be low, and so will be your LH/FSH. Inversely, for AFAB people, taking testosterone will decrease your LH/FSH, and as a consequence, stop or significantly reduce your production of estradiol.
Note
Monotherapy
This type of HRT - that is using only exogenous sex hormones to stop the production of endogenous sex hormones without using any “blockers” - is called monotherapy. You might wonder why this is the common treatment for transmasculine people (usually only taking testosterone), when practitioners are reluctant to prescribe monotherapy to trans women, and usually add androgen blockers with their sackful of side effects. This is mainly due to the fact that, in order to start the feedback mechanism that reduces testosterone, the levels of exogenous estradiol to reach are considered “high” by most practitioners (around 200pg/ml).
As we said before, this is due to the fact that most research on estrogens effects and their link to thrombosis concerns synthetic estrogens used in birth control. Those well-documented and observed side effects of synthetic estrogens are commonly used as the basis science to warn about all estrogens, ignoring (willfully or not?) the research distinguishing synthetic and bioavailable estrogens.
2.5 - Growth hormones
Growth hormone is not a sex hormone. It does, however, play a role in feminization/masculinization during HRT, as it plays a fundamental role during puberty. This page is aiming at informing you about it, and proposing ways to naturally stimulates its production. But it is also a strong warning not to try and take exogenous growth hormones.
A hormonal factor that is not often addressed is the role of growth hormones. As its name states, growth hormone is a key component in tissue growth and repair. It is released in a pulsatile way (at a regular time in the day - actually usually at night during sleep), and its average levels vary in the different stages of life. High during childhood and puberty, they decrease in our twenties. After that, their levels are dependent on the needs: spurts will occur after body traumas in order to stimulate healing, or after intense physical activity (which actually creates many little muscle traumas). In the frame of medical transition, you could compare the role of growth hormones to the role of building workers when sex hormones are the architects. Sex hormones decide what and where to build, growth hormones do the actual building.
The age-related factor explains why starting hormone therapy at younger age (before or in the early twenties) usually leads to faster and stronger development.
Warning
This information, however, should not be read as an encouragement to find growth hormones online and start taking them. This is a very bad idea, for so many reasons. Not only does it constitute a serious health hazard, but if you’re taking it to enhance feminization, you might just reach the opposite effect, as exogenous growth hormones can cause a disproportionate “thickening” of the face (nose, eyebrow, chin…) - even in comparison with typical male features (in case some transmasc people would think this sounds nice)What you can do, however, is to aim at adopting a lifestyle that will naturally stimulate the production of growth hormones. Such lifestyle includes:
- Relatively intense exercise (i.e. is “intense” an exercise the day after which you feel pain in your muscles)
- Sleeping (avoid sleep deprivation, and get as much sleep as possible)
- High protein intake (plant-based protein is protein too).
- Low sugar intake
Sources
Growth Hormone-Releasing Hormone: Clinical Studies and Therapeutic Aspects
Reciprocal interactions between the GH axis and sleep
Human growth hormone response to repeated bouts of aerobic exercise
2.6 - DHEA and intracrinology
DHEA is the hormone found in largest quantity in the human body. It has a very weak masculinizing effet in itself, but its action is mostly due to its conversion into testosterone and DHT in and by target cells. Intracrinology is the subfield of endocrinology who looks at this phenomenon, and it can matter to us (mostly transfem people) for a number of reasons.
As we have explained, most of our sex hormones are produced in our gonads: ovaries and testes. That means that in case of surgical removal of the gonads (orchiectomy/vaginoplasty, ovariectomy…), the vast majority (95%) of our sex hormones circulating in the body will be gone. This also means that after such surgery, transfem people on HRT could stop taking anti-androgens.
However, does suppressing our gonad-produced sex hormones really means the end of all masculinizing/feminizing effects of endogenous hormones?
Not exaclty. And this is where intracrinology and DHEA enters into the game.
Intracrinology is a subfield of endocrinology developped in the 1980s. In the framwork of sex hormones, it is mostly based on the activity of DHEA. DHEA is a hormone massively produced in small glands situated right above the kidneys, called adrenal glands. They produced a bunch of other stuff (including small amount of testosterone and estrogens directly).
Intracrinlogy figured out that DHEA (that makes for the most present hormone in the body) travels to target cells (such as skin, hair follicules, prostate cells…) and is converted there, on the spot, by those very cells, into testosterone and DHT. That means that there is a peripheral production of androgens: not in the gonads, but direclty in the target cells. And what matters is that these androgens will actually direclty activate the androgen receptors in the target cells that has just produced them. After that, they will be metabolized and realeased into the bloodstream as something else. Research has shown that surgical or chemical castration (i.e. by GnRHa) in AMAB people leads to an approximately 50% drop of androgens in the target cells of the prostate. That is far from the 95% reduction observed in the bloodstream androgen levels. And this is likely to be true of skin cells, including hair follicule.
Note
Such research have been conducted in the framework of prostate cancer treatment. Indeed, one of the first thing to do to stop the cancer growth is to stop androgen exposition of the prostate. GnRHa are usually used to this intent, but this is were we realized that even after blocking 95% of bloodstream androgens (suppression of gonadal androgens) by chemical or surgical castration, the prostate cells themselves still kept around 50% of their usual androgen levels. This led to the developpment of a combined treatment of GnRHa and androgen receptor blockers (bicalutamide) in order to block the action of ,those 50% of adrogens left, coming from local conversion of DHEA. This combined treatment proved quite successfull.This means two things:
- After a gonad-removal surgery, a masculinzing activity is likely to continue, namely in the prostate (which is not much of an issue for transfem people if you don’t have prostate cancer), but also in the skin and facial hair follicule (more anoying for many transfem), since around only 50% of androgens acting on those cells will be gone. However, if you were not taking an androgen blocker of the receptor blocker category (Bicalutamide) before surgery, this will not affect you much. Indeed, if before surgery you had manage to reduce your androgen level either by monotherapy, or by any other blockers than an androgen receptors blocker such as biculutamide, then your target cells were already affected by the local production of androgens from DHEA.
- The bloodtest values after surgery will not reflect the masculinzing activity happening from and in the cells, since, as we said, the androgens localy produced from DHEA do not leave the cell into the bloodstream before being metabolized into something else. This is why bloodtest results ususally show a 95% reduction of androgen after gonadal production suppression. Your bloodtest results will most likely show near 0 androgen (not actual 0 - which you do not want anyway - since the adrenal gland also direclty produces a small amount of androgens that is released into the bloodstream).
I speak here of “masculinizing activity”, and of the consequences of DHEA activity for transfem people, because the conversion of DHEA in the skin cells goes only towards androgens. AFAB people will also sythetise androgen in their skin cells from DHEA. In other words, skin cells are only equipped, in every people, to locally sythetize androgens. The vaginal cells, however, will locally produce estrogens from DHEA (which is why DHEA becomes a central hormone for people postmenopause, as it becames the main source of estrogens for the vaginal tissue.)
It is commonly observed a rise in andrenal activity in the few weeks following gonad-removal surgery. DHEA is increased, which leads to masculinzing effects (acne, facial hair growth…) for AMAB people after orchiectomy/vaginoplasty.
This data leads to reconsider the affirmation that an adrogen blocker is useless after surgery. This is true of most androgen blockers that acts - direclty or not - on the levels of the gonads, that is by stopping the gonadal production of androgens. The gonads gone, there is indeed nothing left to block.
However, it makes the case for continuation of androgen receptor blockers, namely bicalutamide, which will be the only solution to block the masculinzing effects of the locally produced androgens, sythetized from DHEA. This is especially true if you were already taking bicalutamide before, without any problem. You could, however, consider lowering the doses. Bicalutamide could prove particularly useful at least in the first few weeks after MTF/MTX bottom surgery, in order to block the effects of the increased activity of the adrenal glands typically observed after removal of the testes.
This also suggests the superiority of bicalutamide (and receptor blockers in general, but you might want to avoid spironolactone for other reasons) as an androgen blocker before surgery, since it is the only one who’s able to block the masculinizing effects of the adrenal activity.
Warning
Note that you should not try to block the adrenal activity itself and reduce the production of DHEA, since DHEA is used in many other steroid conversions that are essential.Sources
Is dehydroepiandrosterone a hormone?
DHEA, important source of sex steroids in men and even more in women
Maximum androgen blockade in advanced prostate cancer: an overview of the randomised trials
3 - Feminizing HRT
This section is dedicated to feminizing hormone therapy. You will find info on estrogens, androgen blockers and progesterone.
3.1 - The different methods
There are different “methods” in feminizing HRT, or medication regimes, whith each their pros and cons. Here are the main ones.
Note
All methods consists primarily in reducing the levels of testosterone. This is critical to an effective HRT since estrogenic feminizizing effects will be blocked if testosterone remains too high. However, it is not advised to remain with low levels of testosterone without complementing by a decent level of estrogens. In other words, if relatively low levels of estradiol (around 60pg/ml) are “sufficient” for feminization if testosterone is brought to near 0, it is not necessarily the ideal situation, and lots of transfem people actually need much higer levels of estradiol to feel good (energy, mood, libido…) This is precisely what many practionners refuse to take into consideration, as they prescribe the minimal dosage of estradiol for effective feminization, but seem to ignore the fact that we also want to be happy and functionning.Monotherapy
As we have described in the “Basic science” section, monotherapy consists in using only exogenous estradiol to reduce the levels of testosterone to target levels, thanks to the negative feedback mechanism.
In other words, you take enough estradiol which does the two things you want: reduce your testosterone, increase your estradiol. Simple enough. Where’s the catch? There is not really any.
Pros:
- Very easy to put in place - take enough estradiol until testosterone crashes down.
- Avoid taking androgen blockers with their lot of side effects
- Higher doses of estradiol usually means better mental health and libido.
- If you are paying for your medication - it can be a cheap option. Both gel and injections are usually cheap.
Cons:
- You have to make sure that you keep your estradiol levels high enough. The threshold to activate the negative feedback is different for each person, but is usually situated around 200 pg/ml.
- Not compatible with all routes of administration, especially oral and patches. Injections are ideal but unavailable through the regular market in many countries, including Sweden. Possible with gel depending on skin receptivity, and using higher doses and/or scrotal method.
Estradiol + progesterone
This could be considered a variation of monotherapy, since the main principle remains the same: using estrogens to naturally reduce testosterone through negative feedback. Adding progesterone can act as a minor complement in case estrogens themselves are not high enough to start negative feedback.
The use of progesterone for feminization, however, is still debated, and its role remains unclear. There are a few things to know in case you decide to take it:
- As we said, it has a small anti-androgen power for AMAB (by negative feedback), but you should not count on it as the only way to efficiently bring down your T. It can be interesting in combination with a relatively high dose of estradiol - as a complement to monotherapy.
- Its role on breast growth is still unclear. Some say it helps from the beginning, but much research suggests it can also limit or block breast growth if taken too soon. The main recommendation is to start after reaching stage 3 of Tanner scale (approx. 2 years of HRT).
- Using oral route (swallowing) results in no effects whatsoever, since the liver first pass will convert and eliminate nearly all of the progesterone. The new converted molecule can cause somnolence and other mood effects, which are actually appreciated by some people. So if you want those effects, you can eat the pill, but it will have, for sure, no effects on breast development and/or testosterone blocking. Otherwise, the best way to reach useful levels is rectal administration, if you get those soft pills. Put one (100mg to 200mg) up your butt before going to sleep.
- In any case, always use bioidentical progesterone, and not synthetic progestogens.
Estradiol + blockers
This consists in using an androgen blocker (blocking either production or reception), in complement to estrogens. There are many androgen blockers, each with different effects and risks. We’ll come back in the next section to all of them in detail. Cyproterone acetate (sold under the name Androcur in many countries) is one of them, even though technically, it is a synthetic progestogen, meaning that its action relies on negative feedback, like monotherapy. Unlike bioidentical progesterone, its antiandrogenic power is extremely strong. However, it doesn’t make it a safe blocker since, unlike bioidentical progesterone, it comes with a bunch of frequent and significant health risks that are common to synthetic progestogens.
Pros:
- You can independently adjust your levels of T and E. (Does not apply to receptor blockers)
- It is the only way to block testosterone if monotherapy doesn’t work for you (insensitivity to gel, or you can’t take high dosage of estrogens…).
Cons:
- You have to make sure that your are not underdosed in estrogens, since being deficient in both sex hormones at the same time can be dangerous (physically and mentally - mainly risks of osteoporosis and depression) NOTE THAT ANDROGEN BLOCKER SHOULD NEVER BE TAKEN ALONE.
- Lots of androgen blockers are known to have annoying if not dangerous side effects. It is the case of Androcur, widely used in Europe.
Dr. Will Power’s method
The main difference is that Power’s research and experience seem to show that putting estrone (E1) into the equation is important. His idea is to start with higher estrone levels for around 6 months by using oral estradiol pills. As we’ve said before, if simply swallowed, most of the estradiol of these pills is converted to estrone. Power claims that this is closer to the hormonal balance evolution in ciswomen puberty, and that initial exposure to estrone helps increase the amount of estrogen receptors. The idea is to prepare the ground for estradiol, which comes after the first 6 months, by maximizing the reception capacities. Introduction of estradiol (E2) after the 6 months of dominantly estrone therapy is realized at high, monotherapy-like dosage (usually injections, sometimes gel). As we said, blockers are sometimes used to complement, as well as progesterone after reaching Tanner stage 3 (around 2 years of HRT).
This initial estrone treatment is what differentiates his method, and also what makes it controversial among healthcare practitioners and the trans community. Indeed, estrone exposure is associated with higher and more frequent risks than estradiol, and Power’s claims of its interest for optimizing the reception of estradiol is still to be proven. Scientifically speaking, Dr Will Power’s method is still considered theory.
3.2 - SHBG: What is it, and why it can matter
SHBG stands for Sex Hormone Binding Globulin. It is present in everyone’s bloodstream, and its amount can matter. Here is what you need to know.
Sex hormones, for the vast majority, don’t run freely in the body. Once they reach the bloodstream, they actually attach to other molecules present in the blood. Most is loosely bound to albumin ( around 54%), another portion is more tightly bound to SHBG (44%). Which leave only 1 to 2% free or “bioavailable” sex hormones. The thing is… only these free estrogens or androgens are active, that is, able to penetrate the cells and produce changes. In other words, albumin, and even more SHBG inhibits the activity of sex hormones.
This can be particularly interesting to know for transfem people using estrogens. Indeed, SHBG levels can vary, and one of the main factors of SHBG increase is…higher levels of estrogens. This mechanism is thought - among others - to be a protection for the pregnant person against the incredibly high levels of estrogens produced during pregnancy, as well the sex hormones produced by the fetus. But in our case it means two things:
-
If your levels of estrogens are good, and you testosterone low enough, but you are not experiencing any (or very little) changes after 6 months of HRT, it might be relevant to measure your levels of SHBG, as some people are born with or develop higher than average levels of SHBG. Do not assume, however, that this is the only explanation for your lack of reactivity to HRT; it is one possible reason among others, and the only way to know is to have your SHBG measured.
-
Theoretically, significantly increasing the dosage of estrogen can be quite useless, if not lead to counter effects, since it might trigger an increase of SHBG, and hence diminishing the levels of bioavailable estrogens. However, this is only how it would work on paper. In reallity, it seems that it would be quasi-impossible (in the frame of trans HRT) to raise your estrogens levels to the point where SHBG levels gets too high and effectively start blocking the feminizing effects of estrogens. You should not worry too much about this issue when going for high-dose estrogens therapy.
To go further - Sources
To read more about it, Transfemscience has a comprehensive article - with numerous sources - on the interactions of sex sormones with SHBG and relevance for transfeminine hormone therapy. It drwas the conclusion that :
“Aside from decreasing free estradiol fractions, increased SHBG levels also decrease free testosterone fractions to an even greater extent. This is advantageous in the case of transfeminine people.
Taken together, lower free estradiol due to increased SHBG levels, whether with non-oral or oral estradiol, isn’t something that should be a major source of concern in transfeminine hormone therapy.”
3.3 - Estrogens
This is a summary of the different estrogen medications used in feminizing HRT. Follow the links below for detailled information on each medication.
Estradiol is the main active estrogen in our bodies, and has a much higher binding affinity than estrone, so that is the one we will use for feminizing HRT. There are also a number of synthetic estrogens, developed by pharmaceutical laboratories in particular for the use in birth control pills: a common one is Ethinylestradiol (EE). As a synthetic derivative of estradiol, EE also comes with more (and more frequent) side effects. This is why it is not recommended to use birth control pills for feminizing HRT. Actually, research has shown that the common side effects of estrogen therapy that trans women are usually warned about by practitioners - and used as a reason to keep them at low doses of estrogens - such as blood clots, are mostly associated to synthetic estrogens (like EE), and to a much lesser extent to bioidentical estradiol.
Target range
A serum level of 200 to 300 pg/ml is usually enough to activate the negative feedback and efficiently reduce the production of testosterone. If are not on monotherapy, the same range also seems to be a target for most transfem people in order to keep a good mood and energy. However, keep in mind that those values can change between individuals, and the best remains to do blood work, and be attentive to how you feel.
This is especially true for the threshold of “overdosing”, which can vary a lot between individuals. Some trans women need higher doses (between 350 and 600 pg/ml) to feel good, when others will have symptoms of overdose at these levels (headaches, nausea, heavy legs). Find what is good for you, when you feel energized, and don’t hesitate to try to get higher levels if you feel symptoms of underdose (tiredness and fatigue, low morale, hot flushes, complete lack of libido…).
Do not assume this is just your mood and do not normalize it. Adjusting your levels CAN make a difference.
Summary of the different routes
| Method | Description | Risks | Access in Sweden |
|---|---|---|---|
| ✅ Transdermal (Gels and patches) | Good method, but results vary between each individual | Very low | Yes, but patches are often out of stocks. Gel has also shown supply disruption recently. Bottles (“Estrogel”) are more convenient than individual small pouches (“Divigel”) |
| ✅ 😐 Oral (Pill) | Not very efficient when swallowed direclty, but good if using sublingual method. Okay for a start, but to be avoided in the long term. Sublingual method is not very convenient. | Medium (increased if swallowed) | Yes |
| ✅ Injections | Very efficient for higher and fairly stable levels, on long term as well | Low (if performed safely) | Not available through prescription; only on DIY |
| 😐 Nasal spray | Good alternative to gel and patch | Very low | Not available |
| 😐 Pellet | Convenient but little data available to assess fully | Low, but risks of multiple scars | Complicated, mostly unavailable |
3.3.1 - Transdermal gel and patches
✅ Transdermal administration (gels and patches) is a safe route, and easily accessible. The main downside is that it can be difficult to reach higher levels of estrogens necessary for monotherapy, and that the levels can vary a lot between individuals.
Estradiol is a good candidate for transdermal administration, meaning that it is rather well absorbed through the skin.
This mode of administration comes in two forms, gel and patches. There is no fundamental difference between the two. The choice is merely a matter of convenience (a daily or twice-daily application of gel, applying the patches once or twice a week). Note, however, that patches are subject to frequent shortages in pharmacies in Europe, and you sometimes need to apply many of them at the same time to reach the levels of estradiol you want, especially if the pharmacy is unable to provide the stronger ones.
In comparison to oral administration, the transdermal way has the advantage of avoiding liver first-pass - that this the quasi-total conversion of estradiol into estrone by the liver after digestion. With transdermal route, estradiol reach the bloodstream directly, without overcharging the liver.
However, there are great inequalities between each individual in terms of skin absorption abilities. Transdermal administration might be very efficient with some, but not with others, who would struggle to reach target levels of estradiol.
Pros:
- Easy and accessible, uninvasive
- Usually gives stable hormone levels if taken with regularity.
- Quite safe in terms of side effects, especially blood-clots (thrombosis)
Cons:
- Doesn’t work great on everybody
- For the gel, you have to let it dry, and be mindful of transfers if you touch people with the skin on which you applied the gel recently
- For the patches: can leave glue marks, irritate the skin, and they tend to fall off in the warm days of summer, with physical activity and warm shower/bath/sauna.
Gel
| Products | Doses | Blood values to monitor |
|---|---|---|
| Divigel, Estrogel (and Lenzetto, not ideal) | 2mg to 8mg a day, spread in morning and evening | Estradiol, Testosterone, FSH/LH (SHBG if you feel no effect after a few months) |
With the gel “Estrogel”, delivered in a bottle with a measured pump, the dosage is usually given in number of pump pressions.
Each pump pression delivers 0,75mg of estradiol; 4 pressions yelds 3mg…
Patch
| Products | Doses | Blood values to monitor |
|---|---|---|
| Estradot | 100 to 400 µg per day | Estradiol, Testosterone, FSH/LH (SHBG if you feel no effect after a few months) |
Equivalence between doses of patch, gel and pills
Theoretically, of 50µg/day patch is equivalent to a 2mg pill, and to 1.5mg in gel. These values, however, can considerably vary. Once again, the best way to ensure good levels is to do blood work.
How to apply gel/patches
Try as much as you can to apply on clean skin to optimize absorption. Apply on a hairless area (shaved works) Do NOT apply on breast: it does not help with breast development, but might increase the risks of breast cancer. Avoid applying on the inner forearm, as it might interfere with bloodworks results. If you do, start applying somewhere else at least a week before testing blood.
Note that a variant of transdermal route is nasal spray (intranasal). Estrogens are absorbed by the mucous membrane of the nose. This route is found to be more convenient by some people. However, this medication is not available in Sweden; but it can be found in other countries.
What is the scrotal method?
Scrotal method consists in applying the gel on the scrotum (the skin containing the testes). This skin being thinner and heavily vascularized, it leads to better absorption, so higher levels of estradiol for a same dose of gel(up to 6 times higher). Research has been conducted, but we know little on the long term effects of this method.
Some trans women using it report increased fragility of the penile skin, with skin easily breaking at points of frictions. Topical application of the gel on this area might also lead to overly low levels of testosterone, which is not recommended. Testosterone is part of a healthy hormonal balance for all individuals, and participates in maintaining cognitive functions such as memory, among other important functions… If, as a transfeminine person, you will want to stay under 0.5 ng/ml (50 ng/dl), reaching absolute zero (or close to it - under 0,8 ng/ml) is not recommended. Some trans women reported that stopping the scrotal method after using it for more than 6 months both improved the skin fragility, and the overly low testosterone level.
It remains, however, a possible method to use in order to achieve higher levels of estradiol with limited gel supply.
Sources
Testosterone replacement in male hypogonadism
« Due to the superficial vascularity of the scrotal skin, there is a 5-40 fold increase in steroid absorption when compared to other skin sites. »
« the relative permeability at other application sites was greatest for the scrotum (42.0), increased for the back (1.7), reduced for the lateral ankle (0.42), and lowest for the sole of the foot (0.14). »
3.3.2 - Oral
✅ / 😐 Oral route (Pill) is generally okay for a start, but should avoided in the long term. Swallowing the pills is overall not very efficient, and leads to excessive levels of estrone, and low estradiol. Sublingual method can correct this, but can be inconvenient.
| Products | Doses | Blood values to monitor |
|---|---|---|
| Femanest, Progynon | Between 1mg and 8mg per day | Estradiol, Testosterone, FSH/LH (SHBG if you feel no effect after a few months), Hepatic enzymes if swallowed (ALAT, ASAT, GgT) |
This is a very common administration route, and easy to take.
We should however distinguish two ways to take an estrogen pill: swallowing and letting it melt in the mouth.
Swallowing
This is the easiest way, but also the one associated with the higher risks for your health, as it increases the risks of thromboembolic accidents. These risks, however, remain relative to each individual, and medication has improved greatly since the first versions of estrogen pills that used to be the norm in the transfem community (Premarin, or conjugated equine estrogens).
As stated above, the pills prescribed for HRT (bioidentical estradiol) remain significantly less risky in regards to thromboembolic events than the synthetic estrogens used in birth control medication. (Source)
The higher risks associated with swallowing are to be put on the hepatic first pass - which is the liver dealing with ingested chemicals when they are digested. This stands for any medication taken orally: all of them will mobilize this liver function, and, so to speak, making it a bit more “tired”. As a general rule, it is best to avoid oral medication when possible.
The second reason is another consequence of the liver first pass, but more closely related to estrogen. We talked about it before: the liver converts the vast majority of the swallowed estradiol into estrone. Not only is estrone associated with higher health risks, but it also significantly less potent in terms of feminizing effects.
Pros
- Easy and accessible
- Usually gives quite stable and long-lasting hormone levels
Cons
- Increases risks for health (mainly thromboembolic accidents)
- Usually give low estradiol levels, and higher estrone levels.
Sublingual/buccal method
This is the alternative to keep the pills, but avoid the hepatic first pass and hence the risks associated. It consists in letting the pill completely dissolve under the tongue, or between the inside cheek and gums (a bit like snuss).
This way, estradiol will be directly absorbed by the buccal blood vessels, and reach your bloodstream without passing first by the liver. This usually leads to a much faster absorption , with much higher levels. However, the levels tend to fall down quite fast as well. This “yoyo” effect usually leads people to take a pill every 8 to 12 hours in order to maintain correct levels.
Pros
- Easily gives higher estradiol levels
- Less thromboembolic risks
Cons
- Yoyo effects - having to take a pill every 8/12 hours
- No scientific research on the possible risks of this method (and the consequences of the yoyo effect on feminization/body development)
3.3.3 - Injections
✅ Injections are a very efficient and safe route, on long term as well, leading to relatively stable and high levels of estradiol. It is safe as long as you perform the injection well, and make sure that the product you use if legit and uncontaminated. The main problem is that their are not available in most european countries, and necessitates DIY competences.
| Products | Doses | Blood values to monitor |
|---|---|---|
| None available through prescription in Sweden | Estradiol Valerate : 4 to 7 mg every 5 days / Estradiol Cypionate : 6-7 mg every 7 days or 10-11 mg every 10 days / Estradiol Enanthate : 7.5mg every 7 days or 10-15 mg every 14 days | Estradiol, Testosterone, FSH/LH, SHBG |
Injections of estrogens are not very common in Europe. It is, however, a much more common administration route in other countries, namely in the USA, Latin America, and Japan.
Injection - if you don’t have issues with needles - is a very convenient way to reach high levels of estradiol for monotherapy. It allows for longer time between intakes (up to 15 days with estradiol enanthate). It is also relatively cheap as a vial bought on the grey market costs between 55 and 75 $ USD and can usually last for a year (between 4.5 and 6.5 $/month).
Injections are typically performed as Intramuscular or Subcutaneous. It works by leaving a depot (a small reserve) in the muscle or fat tissue. The depot will slowly release the products, which will enter the bloodstream gradually.
We give more detail on the dedicated pages on how to perform those two types of injections.
What is good to know here is this:
- Intramuscular injection means injection inside the muscle tissue. It usually means using a longer needle, which can be a bit more painful and more uncomfortable if you don’t like needles. The muscle tissues being more vascularized, absorption is faster.
- Subcutaneous injections means injecting between the skin and the muscle, in the fat layer. We usually choose a spot with more fat (upper butt…). With less blood vessels, absorption of the depot in fat tissue is slower, which allows for even longer time between injections, and more gradual increase of the levels after injections.
Esters – What are they?
Injections come with slightly different molecules, which will have a consequence on absorption speed and levels of estradiol reached per shot (and hence, the frequency and doses of each injection). What we use for estrogen injections is called an ester.
An ester designates a molecule (here estradiol) that has been esterified; meaning it has been slightly modified by an addition/replacement of a chain of atoms. This technique is used in many medications, in the objective of optimizing the bioavailability of the drug (and how efficient it is in our system). In a way, the idea is to anticipate the fact that after intake, the body will metabolize the molecule into a weaker (or just very different) form. Esterification creates what we call a “prodrug”: an inactive drug taken as such, but that will become active after its metabolization by the body.
Imagine you want to take a molecule we simplify as “AB”. If you take it just like that, the body will metabolize AB into A, and it won’t be exactly what you want. Esterification consists in first turning AB into ABC; then, after ingestion or injection, the body will then metabolize ABC into AB, and you’ll end up with what you want. For this reason (because estradiol esters are metabolized into estradiol), estradiol esters are considered bioidentical estrogens and not synthetic. The active molecule acting on your body remains, at the end, estradiol (E2).
The main esters used for injections are, Estradiol valerate, Estradiol enanthate and Estradiol cypionate.
Estradiol valerate usually leads to a fast and high peak, falling down rather quickly as well. It means more frequent injections, and also a bigger span between high and low (unstable levels)- which can affect your mood. (Note that estradiol valerate is also used for the oral pill Progynon)
Estradiol enanthate gives slightly lower levels (though still high compared to other routes), but lasts longer. This allows for more stable levels, and the possibility to space out injections (once a week for best stability, up to once every two weeks).
Estradiol cypionate behaves similarly with again slightly lower levels.
You can refer to this Injectable Estradiol Simulator, but keep in mind that data is sometimes scarce, and your actual levels can vary greatly. The best remains to check your levels with blood work, and listen to your body and mind.
Pros
- Easily gives high levels of estrogens
- Allows for easy monotherapy and hence avoid androgen blockers
- Lower risks than with oral route
- No difference of absorption between individual (everyone is receptive)
Cons
- Can produce unstable levels (but can be corrected by dose/frequency adjustments)
- Impossible to get through the legal/prescription market.
- It’s an injection (needle fear…)
Please refer to the dedicated page for details about practicing safe injections.
3.3.4 - Pellets
😐 Pellets are a very convenient option, but little data is available to assess fully, and is very seldom proposed by practitioners. Most estradiol pellets are pescribed to AFAB people as a contraceptive.
This is a rare solution, mainly used in Australia. It consists of a pellet implanted under the skin, delivering estrogens steadily and regularly. This route is also used as a contraceptive method, with a different estrogen. The implantation can leave a little scar, and considering the pellet has to be changed after a few months, it is not ideal to have this route as a long term solution - especially if you started HRT early in your life. That is why it is mostly proposed to post-menopausal women.
Pros
- Delivers steady levels of estrogens, and once in place, you’re good to go for a few months, without having to remember to take your medication
Cons
- Can leave scars, accumulating with years
- You need to see a doctor everytime you change it
- Can sometimes (though rarely) “detach” and circulate in the body (and is sometimes lost)
- You can’t be sure the dosage will be optimal before you put it, and then have to wait a while before correcting it if it is not.
3.3.5 - Sources on the risks of thrombosis
Patients are usually warned about the risks of thrombosis - deep vein thrombosis and thromboembolic events. This pages gives a number of articles whose conclusions show a few things:
- Risks depends on the administration routes: transdermal and injections are safer than oral
- Risks depends on the type of estrogens: synthetic and non-bioidentical should be avoided
Transdermal delivery of bioidentical estrogen in menopausal hormone therapy: a clinical review
Pharmacology of estrogens and progestogens: influence of different routes of administration
Menopausal hormone therapy and venous thromboembolism
Oral Contraceptives and HRT Risk of Thrombosis
Orchidectomy versus oestrogen for prostatic cancer: cardiovascular effects.
Therapy Insight: parenteral estrogen treatment for prostate cancer—a new dawn for an old therapy
3.4 - Androgen blockers and progestogens
This is a summary of the different antiandrogen medications used in feminizing HRT. Follow the links below for detailled information on each medication.
In order for estrogens to be efficient, the action of testosterone MUST be blocked, one way or the other.
If monotherapy does not work for you, the solution can lie in anti-androgens, or androgen blockers - sometimes only refered to as blockers. Blockers actually encompass a great variety of medications, working in differents ways.
It is usually considered that orchiectomy or vaginoplasty allows for stopping anti-androgens, but not estrogens. It is in reallity a bit more complicated, and you can refer to the page on DHEA and intracrinology to know more about this issue.
Summary table of androgen blocking alternatives
| Name | Description | Risks |
|---|---|---|
| ✅ Monotherapy | High dose estrogen without blockers - uses the negative feedback mechanism of the body | Low increase of thromboembolic events, especially with very high doses. |
| ✅ Bicalutamide | Very efficient androgens blocker. Blocks the reception of androgens. | Low - but monitoring of liver fuction remains important |
| ✅ GnRHA | “Puberty blockers”, but can be used by transfem of any age to block the production of androgens. Usually delivered as injectable, sometimes nasal spray | Low |
| 😐 Spironolactone | Diuretic with an anti-androgen side-effect | Risks of hyperkalemia (excess of potassium, with variable risks), and reduced blood pressure |
| 😐 Progestogens (others than Androcur) | Very commonly prescribed anti-androgens. Work on the same basis as monotherapy, but with more side effects. | Risks of depression, hyperprolactinemia and liver failure |
| ❌ Finasteride | Useful against “male pattern hair loss”, otherwise not very efficient | Risks of depression and neurological problems |
| ❌ Dutasteride | Useful against “male pattern hair loss”, otherwise not very efficient | Risks of depression and neurological problems |
| ❌ Androcur | A very commonly prescribed synthetic progestogen, officially unadvised by many countries | Risks of depression, meningioma (meninges tumor) and liver failure |
| ❌ Flutamide | Obsolete medication (discontinued in Sweden) | High risks of liver failure. |
We can sort androgens blockers in 4 groups, according to their mode of actions:
- Androgen receptor blockers (Bicalutamide, Spironolactone)
- GnRH agonists and antagonists (also called Puberty blockers)
- Inhibitors of 5a-reductase (Finesteride, Dutasteride)
- Progestogens (among which Cyproterone Acetate or Androcur) We will now go through all of them, group by group.
3.4.1 - Androgen receptor blockers: Spironolactone and Bicalutamide
Spironolactone and Bicalutamide are two androgen receptors blockers used in feminizing HRT.
If spironolactone is more widely prescribed, bicalutamide should be preferred.
Since they block the reception and not the production, no decrease of androgen levels will be shown on the blood test result.
Androgen receptor blockers are molecules which have the capacity to bind to the androgen receptors. Remember the image of the key and keyhole? Androgen receptor blockers are like keys that fit in the keyhole, but can’t open it. And not only it can’t open it, but it’s stuck in there so that the keys that could actually open it can no longer get in. So, a bit like when your key breaks in the lock before you open the door…
What this also means is that what is blocked is the reception of androgens (and hence their effects), but not the production.This doesn’t make them less effective. If your levels of estrogens are not blocking the production of testosterone (which would be the reason you want to take androgen blockers), then testosterone will still run in your system, and you will still see it on the blood test results. This doesn’t mean the treatment doesn’t work, and you should judge this by the results you feel and observe on body changes.
The main drugs in the category are Spironolactone and Bicalutamide. Flutamide is a sort of earlier and much more risky version of bicalutamide, and it has been removed from the market in many countries.
😐 Spironolactone
This is actually a diuretic medication in the first place (i.e. intended to make you pee). Its anti-androgenic function is one of its secondary effects. In addition to working as a receptor blocker, it also has a small 5a-reductase inhibition power (prevents conversion of Testosterone into its more potent form DHT - read more in the dedicated section).
One issue is that it also blocks other receptors, mainly the ones of progesterone, and cortisol, which can lead to undesired effects.
The main issue reported by transfem people using it is its diuretic effect.
It also comes with risks of hyperkalemia, which is an excess of potassium. This can have dangerous consequences on cardiac health. For this reason, you might want to monitor your diet, keeping an eye on your potassium and sodium intake.
Finally, many report poor efficacy as an androgen blockers. All of the above gives a pretty bad reputation to spironolactone in the trans community, but it remains a widely prescribed drug in feminizing HRT - especially in the USA.
| Products name in Sweden | Dose | Blood values to monitor |
|---|---|---|
| Spironolactone (sometimes Aldactone in other countries) | Between 50 and 200 mg per day | Potassium, Sodium, ALAT, ASAT, GGT |
Pros
- Convenient and usually cheap
Cons
- Limited efficacy
- Makes you pee
- You might need to monitor your diet to avoid potassium excess
✅ Bicalutamide
As opposed to spironolactone, bicalutamide has been conceived as a pure androgen blocker in the first place, in order to treat prostate cancer, and later on hirsutism, and as a puberty blocker. It blocks the reception of androgens in a very efficient way, without blocking other receptors, hence limiting the secondary effects. It is increasingly considered one of the best alternatives among androgen blockers, along with GnRHa.
A study showed that it has feminizing effects by itself, as the testosterone running in the body without finding a place to bind is eventually aromatized into estradiol, giving higher estradiol levels than when testosterone finds and binds to its receptors. However, it is safer to never take an androgen blocker by itself, and always add estrogens.
| Products name in Sweden | Dose | Blood values to monitor |
|---|---|---|
| Bicalutamide, Casodex, Bicalustad | 25 to 50mg a day | ALAT, ASAT, GGT |
Pros
- Very efficient
- Nearly no secondary effects and low risks for health
Cons
- Sometime a bit expensive
- Practitioners are a bit reluctant to prescribe (because uniformed)
- You have to monitor your liver health (though the risks remains considerably lower than with synthetic progestins like Androcur)
About the risks of liver failure
Taking bicalutamide often comes with warning of liver failure. If this risk exists, it should, however, be relativized. This risk remains extremely rare: in 15 years of existence and usage, the drug has led to 14 reported cases of liver failure in the world.
A study on 4052 prostate cancer patients taking 150mg of bicalutamide daily showed that only 3.4% of the patients developed abnormal levels of liver enzymes. In comparison, we find the number rising to 10 or even 20% for people treated with Androcur (cyproterone acetate). Besides, in feminizing HRT, the common dosage is 50mg a day.
As a safety measure, the best remains to regularly monitor your liver enzyme levels: ALAT, ASAT, GGT. You can see an increase of them in the first few months of the treatment, which usually resorbs after a while.
Besides, remain attentive to symptoms of fulminant hepatatis (fatigue, nausea, abdominal pain, jaundice, confusion…)
About the cardiovascular risks
If your practitioner is reluctant to prescribe bicalutamide for you, invoking cardiovascular risks, this is known to be a conclusion inferred from a different case. Nothing shows that bicalutamide brings, by itself, cardiovascular risks. Those risks are inferred from the cases of cis-men in treatment for prostate cancer. Those patients end up with sex hormone deficiency, since they do not complement with estradiol intake. It is sex hormone deficiency that bears increased risks of cardiovascular diseases; these risks do not concern transfem people compensating with estrogens.Dosage
A dosage of 50mg/day is usually sufficient. If your testosterone has already been lowered with negative feedback, half this dose can be enough to block the leftovers of testosterone (take one 50mg pill every other day). If you feel masculinising effects coming back, return to 50mg/day. Theoretically, 50mg of bicalutamide can block around 200 ng/dl of testosterone (1mg of bica blocks 4ng/dl).
Keep in mind that it will not affect the levels of testosterone shown in the blood test results. This is absolutely normal.
More resource on bicalutamide
General information articles on bicalutamide :
- Bicalutamide – Wikipedia
- Medical uses of bicalutamide – Wikipedia
- Side effects of bicalutamide – Wikipedia
- Pharmacology of bicalutamide – Wikipedia
- Comparison of bicalutamide with other antiandrogens – Wikipedia
- FAQ par transfemscience.org
Specific sections with information on bicalutamide (and other nonsteroidal antiandrogens) in transgender women :
- Medical uses of bicalutamide § Transgender hormone therapy – Wikipedia
- Transgender hormone therapy (male-to-female) § Nonsteroidal antiandrogens – Wikipedia
- Flutamide § Transgender hormone therapy – Wikipedia
- Nilutamide § Transgender hormone therapy – Wikipedia
- Specific sections with information on bicalutamide (and other nonsteroidal antiandrogens) in cisgender women :
- Medical uses of bicalutamide § Skin and hair conditions – Wikipedia
- Bicalutamide § Research – Wikipedia
- Flutamide § Skin and hair conditions – Wikipedia
- Nilutamide § Skin and hair conditions – Wikipedia
Specific sections with information on bicalutamide in boys with precocious puberty (potentially relevant to the use of bicalutamide as a puberty blocker in adolescent transgender girls) :
- Medical uses of bicalutamide § Male early puberty – Wikipedia
Scientific Literature
- Relevant literature excerpts on bicalutamide in transgender women
- Care of Transsexual Persons (Gooren, 2011)
- Bicalutamide as an Androgen Blocker with Secondary Effect of Promoting Feminization in Male to Female (MTF) Transgender Adolescents (Neyman, Fuqua, & Augster, 2017)
- Bicalutamide as an Androgen Blocker With Secondary Effect of Promoting Feminization in Male-to-Female Transgender Adolescents (Neyman, Fuqua, & Eugster, 2019)
Literature reviews on bicalutamide (and other nonsteroidal antiandrogens)
- Bicalutamide § Further reading – Wikipedia
- Bicalutamide / Nonsteroidal Antiandrogens – PubMed (filter search results by « Review » in the left-hand column)
Regulatory Body Materials
- Casodex (bicalutamide) 50 mg FDA (US) label
- Casodex (bicalutamide) 150 mg MHRA (UK) prescribing information
- Casodex (bicalutamide) 150 mg MHRA (UK) patient leaflet (PDF)
- Casodex (bicalutamide) 50 and 150 mg MHRA (UK) public assessment report
- Bicalutamide (Casodex) as an Antiandrogen for Transgender Women Megathread
- Bicalutamide frequently asked questions (FAQ) and common misperceptions
- Scientific Literature about Bicalutamide
- Hormone Therapy for Transgender Women 101 – u/Alyw234237
- Recent Study: Bicalutamide in MtF Adolescents (value as an AA and for promoting feminisation) – u/Ambrosia25
- Calculation and discussion of bicalutamide dosage potentially required for puberty blocking in MtF trans girls – u/Ambrosia25 (direct link to the document/email being discussed here)
- Rise in blood levels of bicalutamide for various dosages (graph) – u/Ambrosia25
- Indirect evidence that bicalutamide is able to provide the same benefits as flutamide for scalp hair loss – u/Ambrosia25
- A ranking of AAs in terms of Safety, Effectiveness, Tolerability and Cost (inexpensiveness) – u/Ambrosia25
- New publication: Bicalutamide as an Androgen Blocker With Secondary Effect of Promoting Feminization in Male-to-Female Transgender Adolescents (Neyman, Fuqua, & Eugster, 2019) – u/Alyw234237
- Hormone Therapy for Transfeminine Non-Binary Individuals and Femboys 101 – u/Alyw234237
News and Blogosphere
- Bicalutamide, a new anti-androgen for trans women and girls (Jones, 2018)
⛔ Flutamide
It is considered an “ancestor” of bicalutamide. It works the same way, but with much more risks and side effects, especially on liver function. It should NOT be prescribed by any practitioner, and has been put off market in many countries.
3.4.2 - Inhibitors of 5a-reductase: Finasteride and Dutasteride
❌ Finasteride and dutasteride work by inhibiting the transformation of testosterone into its more potent form DHT. They will only achieve one thing: put your health at risk, without any benefits in terms of feminization. They are strongly unadvised and should be avoided at all cost.
5a-reductase (5 alpha) is an enzyme responsible for the conversion of testosterone into its much more potent form DHT (dihydrotestosterone). The particularity and mode of actions of this group of medication is to inhibit the production of this enzyme, and hence blocking the conversion of T into DHT. DHT is considered to have masculinizing effects up to 10 times stronger than testosterone, and it is the main hormone responsible for hair loss (sometimes called “male pattern hair loss”). This is why the medications of this group (Finasteride and Dutasteride), are most commonly prescribed to cis-men seeking to reduce hair loss.
One problem is that the enzyme 5a-reductase is responsible for at least 9 other conversion reactions in the synthesis of steroid hormones. Consequently, inhibiting it does not only affect the conversion of testosterone to DHT.
An other problem is the medication won’t affect the levels of testosterone (the portion of T that would have been converted into DHT will remains as… testosterone), which will still run in the bloodstream, reach its receptors unhindered, and lead to masculinizing effects. This is why these medications will in no way be enough to block androgenic activity, and allow for feminization. It is only useful to reduce hair loss, and the best remains to consider another option to actually block the effects of testosterone (production or reception). Besides, low testosterone also means low DHT, since there is no testosterone to convert! This is how absurd the prescription of these medications is.
By opting for another blocker, you will find two benefits: Actually achieve better feminization, since with 5a inhibitors alone, your testosterone levels will remain unchanged. Avoid the negative side effects of the 5a inhibitors. These mostly come from the fact the 5a-reductase is also responsible for many other hormones synthesis, whose perturbation can cause anxiety, depression, suicidal ideation, neurological diseases and loss of libido.
The only reason to consider finasteride/dutasteride is if you managed to significantly reduce your testosterone by another way, but you still seem to be affected by hair loss, and you show abnormaly high levels of DHT on the blod tests. And considering the side effects, this decision should not be taken lightly.
Finasteride
Warning
❌ Unadvised : Risks of depression and neurological problems.Conceived for cis-men preoccupations: to reduce the levels of DHT (and hair loss associated) while keeping high levels of testosterone.
If you do not have abnormally high levels of DHT despite reducing your testosterone, taking finasteride is only taking unnecessary risks, without any benefits!
| Products name in Sweden | Dose | Blood values to monitor |
|---|---|---|
| Finasteride, Propecia, Prosterid | 0.25 to 2mg a day | Testosterone, ALAT, ASAT, GGT |
Finasteride is at the origin of the healthcare scandal called “Post-Finasteride Syndrome”. This “syndrome” is a set of effects such as anxiety, depression, suicidal ideation, neurological diseases and loss of libido. If this syndrome strikes a minority of finasteride users, they can be permanent, and persists after stopping the treatment.
Dutasteride
Warning
❌ Unadvised : Risks of depression and neurological problems.All what we said of finasteride is true of Dutasteride. The only difference is that dutasteride is able to prevent even more efficiently the conversion of testosterone into DHT.
| Products name in Sweden | Dose | Blood values to monitor |
|---|---|---|
| Dutasteride, Avodard | 0.5mg a day | Testosterone, ALAT, ASAT, GGT |
3.4.3 - GnRH agonists and antagonists (“Puberty blockers”)
- GnRH agonists and antagonists are safe and very efficient androgen blockers. They block the production directly at the higer level of the hypothalamic–pituitary–gonadal axis.
- The main difference between agonists and antagonists (besides the price) is the initial peak of testosterone that is observed with agonists.
- Since they block the production of endogenous sex hormones at the higher level of the chain, they can be used by transmasculine people and AFAB people who want to block theiy production of estrogens.
- They are the medication refered to as “puberty blockers”, but can be used at all age.
Agonists and antagonists of GnRH (Gonadotropin Releasing Hormones) are mostly known by most people as the “puberty blockers” proposed in some countries to minors, before adding exogenous sex hormones. But blocking puberty means nothing else than to block the production of endogenous sex hormones. Consequently, GnRHa can be used as a very efficient androgen blocker for all transfem people (as well as transmasc people)
They have mostly been conceived to treat hormone-dependent cancers (breast, prostate), but also as puberty blockers for cisgender children who show signs of puberty at an age considered too early. In this respect, it is good to notice that the medication has been given to cisgender children without any protest and concerns, but it has become a public health debate at the moment it was used for trans children/teens.
In practice, they work by blocking the production of testosterone at the very early stage of the process. We make the distinction between GnRH antagonists and GnRH agonists. Both work at the same level of the production chain, but in opposite ways; but both reach the same goal, and have the same effect - nearly total shutdown of testosterone production.
Sex hormone production is controlled by the levels of FSH and LH. The production of these is itself controlled by pulsatile release of GnRH. The idea of the medication is to reduce the levels of FSH/LH and hence of testosterone; this is where the distinction between antagonists and agonists is important.
-
GnRH antagonists will reduce FSH/LH by blocking the reception of GnRH by the pituitary gland, which then doesn’t get the order to produce FSH/LH. They work on the pituitary gland’s GnRH receptors the same way bicalutamide works on the body’s androgen receptors: the broken key in the lock, which can’t be opened anymore. A GnRH antagonist available in Sweden is Degarelix (Firmagon), but is nearly exclusively prescribed for cancer treatment.
-
GnRH agonists work by over stimulating the pituitary gland, which, after a phase of high production of FSH/LH (and hence a peak of testosterone of about a week), will stop reacting to GnRH, and hence the whole sex hormone production will shut down. Common GnRH agonists (the most commonly prescribed because cheaper) are Triptolenin (Gonapeptyl) and Leuprorelin (Eligard, Enanton, Procren). Usual doses of 3mg/month or 11.5mg/ 3 months.
A peak of testosterone will start around the 3rd day after the first injection. It will last around a week and does not repeat afterward on the next injections. Some people use bicalutamide in order to counter the effects of testosterone during this peak phase.
They are all quite safe, with nearly no side effects, and great efficacy. Their main problem is that they are usually quite expensive, making them difficult to access if you don’t have health insurance, or just hard to get prescribed because practitioners will tend to favor cheaper alternatives. Besides, they mostly in the form of injections, given every month or every 3 months.
A nasal spray exists (Nafarelin, sold under the brand name Synarel) which can be a good alternative for people who prefer to avoid injections.
3.4.4 - Synthetic progestogens (Androcur...)
- This sections concerns progestogens in general and synthetic progestogens, as used as androgen blockers.
- For information on bioidentical progesterone, refer to the dedicated page.
- Androcur (cyproterone aceate), the main synthetic progestogen used in feminzing HRT, is strongly unadvised by most trans organizations (but not the WPATH), and should be avoided if possible.
Progestogens is the third group of sex hormones after androgen and estrogens. We will differentiate here between “natural” (bioidentical) progestogens (progesterone is the main one) and synthetic progestogens, developed by the pharmaceutical industry for different purposes (namely contraceptive medications, and anti-androgen medications).
Progestogens’ main function, for ciswomen and AFAB people, has to do with ensuring the means and continuation of pregnancy: regulate the cycle, maintain the endometrial tissue of the uterus during and after ovulation, allow lactation…
For transfem people, only the secondary effects of progestogens are of interest. Those effects includes:
- Reduces the production of testosterone (anti-androgen)
- May help finalize breast growth by developing terminal lobules necessary for lactation.
- May terminate/limit breast development if taken before Tanner stage 3.
- Can cause the chest to swell.
- May alter water retention by the body.
- May increase appetite.
- May promote fat accumulation and weight gain.
- May increase metabolism.
- May promote sleep.
- Can increase or on the contrary decrease the libido.
- Can limit or on the contrary aggravate hairiness
- May cause drowsiness and dizziness (only for progesterone).
- May increase the sensation of dysphoria.
- May increase the risk of depression.
- Increases the risk of breast cancer (particularly for synthetic progestins).
Most of the negative effects given above are associated with synthetic progestogens.
Synthetic progestogen:
So, why would you take synthetic progestogens? Because they can work as very efficient anti-androgen, thanks to the natural negative feedback: more of any sex hormones leads to less of endogenous sex hormones. To the body, a synthetic progestogen is read as any other sex hormones: enough of it will start the negative feedback mechanism.
This is true of bioidentical progesterone and synthetic progestogens. The difference being that bioidentical progesterone has a weak effect of negative feedback (you would need a lot to start it), when synthetic progestogens have been developed in order to have a very strong effect as they last much longer in the body.
Androcur
Warning
⛔ Unadvised : Risks of meningiomas, prolactinenia, liver failure, depression…The most potent and widely prescribed synthetic progestogen is Cyproterone Acetate, sold under the name of Androcur. The use of Androcur is banned in the US because of its risks of liver failure, in favor of Spironolactone. In the UK, GnRHa are largely prefered. Androcur remains the most prescribed anti-androgen medication in Europe.
Androcur accumulates the strong anti-androgenic effect through negative feedback, with a small androgen receptor antagonist, plus all progesteronic effects - especially those of synthetic progestogens. It carries a load of adverse side effects, namely prolactinemia (possibly leading to bone problems) and meningiomas (tumor of the meninges). In some countries, like France, a doctor cannot prescribe Androcur without written consent of the patient, and regular MRI scans.
It is also associated with liver failure, and depression.
If you cannot access another medication, you should try to limit the doses as much as possible. Studies have shown that Androcur reaches its maximal effect at 10mg/day. It is unnecessary to exceed this dose, and that would only expose you to more risks.
| Products in Sweden | Dose | Blood values to monitor |
|---|---|---|
| Androcur | 6 to 10mg/day | Testosterone, LH/FSH, ALAT, ASAT, GGT, Prolactine, B12 Vitamin |
Pros:
- Very efficient anti-androgen
- Stronger progesteronic action than bioidentical progesterone
Cons:
- Important risks of depression
- Associated with drastic fall of libido
- Risks of prolactinemia, liver failure, meningiomas
- Might perturb breast growth if taken before Tanner stage 3
Androcur is one among many synthetic progestogens. All the others have their bunch of undesired side effects, mostly - at different degrees - depression, liver failure, and prolactinemia. Those drugs include Levonorgestrel, Dydrogesterone, MPA, Norethisterone…
3.5 - Progesterone
This article concerns only bioidentical progesterone. You can read more on progestogens in the anti-androgen section. We decided to create another section for bioidentical progesterone since it is mainly used as an addition to a treatment and not as an anti-androgen.
Progesterone has relatively few and minor effects on the body, compared to estrogens. Its effects and secondary effects are, besides, still debated among the trans community and medical practitioners and researchers; and the observed effects are sometimes contradictory. If you decide to start taking progesterone, try to be attentive to how it makes you feel, and stop if you feel negative effects as it will most likely affect you more negatively than positively.
Considering that the scientific community seems undecided on the fact that it helps with breast growth (and shaping), and that it could also hinders breast developpement if taken too soon, our recommendation remains to avoid this risk by waiting to reach stage 3 of Tanner scale before taking progesterone.
Start gradually with 100 mg, and consider increasing to 200 mg if you notice positive changes, and/or it helps with your mood.
As opposed to synthetic progestogens, bioidentical progesterone has a very short half-life (the measure to count how long the molecule is active in the body before metabolization/evacuation). In barely a few hours, swallowed progesterone is entirely eliminated by the body.
Besides, when taken orally, progesterone is nearly completely metabolized into allopregnanolone (and to a lesser extent other molecules). This can be responsible for psychoactive effects, similar to low doses of alcohol: somnolence and drowsiness, slight euphoria and relaxation, vague sensation of “being high”. If this can be a disturbance by some, others actually enjoy those effects, especially in cases of insomnia, as taking the progesterone capsule orally right before going to bed might help.
If you seek the actual (possible) effects of progesterone (possible help with breast development and shaping…), the rectal way is the best. Several progesterone medications (Utrogestan, Luteus) presents themselves as a soft capsule or pill that can be inserted in the vagina. In a lack of vagina, the rectal tissue will work similarly. If you got a vaginoplasty, keep using the rectal way as the neovaginal tissue (penile skin in most cases) won’t be as absorbent as the rectal mucous tissues. In practice, simply insert the capsule in the rectum before going to bed. Diffusion will last longer, and the progesterone won’t be eliminated as quickly and metabolized into allopregnanolone.
Some practitioners prescribe topical progesterone as a gel, to apply directly on the breast. If topical application of estrogens on this area is very unadvised (it might only increase the risks of breast cancer), the same technique with progesterone does not seem to cause this problem, and instead enhances breast development. Keep in mind that the technique remains experimental, and mostly practiced in the US by Dr Will Powers, whose method (with its limits) are described here. Besides, topical progesterone gel is not directly available in Sweden, and access to it is conditioned by a practitioner and a pharmacy willing to prescribe and produce a compounded drug for you. However, some DIY suppliers propose progesterone gel.
These are the main possible effects of progestogens:
- Those effects includes:
- Reduces the production of testosterone (anti-androgen)
- May help finalize breast growth by developing terminal lobules necessary for lactation.
- May terminate/limit breast development if taken before Tanner stage 3.
- Can cause the chest to swell.
- May alter water retention by the body.
- May increase appetite.
- May promote fat accumulation and weight gain.
- May increase metabolism.
- May promote sleep.
- Can increase or on the contrary decrease the libido.
- Can limit or on the contrary aggravate hairiness
- May cause drowsiness and dizziness (only for progesterone).
- May increase the sensation of dysphoria.
- May increase the risk of depression.
- Increases the risk of breast cancer (particularly for synthetic progestins).
3.6 - Maintaining erections and healthy penile tissue: topical testosterone
Feminizing HRT will most likely cause a decrease - if not loss - of erections, and primarily spontaneous erections. If this comes with joy and helps with genetital dysphoria for many, some might want to prevent this phenomenon, for different results: desire to maintain sexual practices that requests erections, or avoiding as much as possible penile tissue atrophy.
Indeed, spontaneous erections are a way for the body to keep the penile skin and inner tissue elastic and resilient to friction and minor wounds. With the disappearance of androgen impregnation in these tissues, you might experience pain during erections, and more fragile skin. As described here, the scrotal method of applying gel seems to increase this phenomenon.
Warning
There is no scientific consensus on this, and present knoweledge comes exclusively from individual practionners and patients willing to experiment.“This cream is applied topically to the penis/scrotum once a week at bedtime in AMAB people experiencing erectile dysfunction, painful erections, tissue atrophy (shrinkage and thinning of the skin). It is used with an escalating frequency approaching SRS for optimal tissue health. Post SRS it can be used weekly during a dilation session (by coating the dilator) and sometimes can help achieve additional depth due to increasing tissue elasticity.” “This can be done without increasing systemic levels or causing re-masculinization if you use my compounded formulation, which is 1 gram of compounded 0.5% topical testosterone topically to the penis and scrotum once weekly. It tends to raise T levels about 10-20ng/dl with weekly administration.”
If you manage to have it prescribed, you will most likely need to get the medication compounded for you, as the weakest gel available in Sweden has a 1.62% concentration, when what Dr Powers suggests is a 0.25% to 0.5 % concentration (2.5 mg to 5mg/g).
3.7 - That was a lot... So, what should I take?
Our goal is to have you be able to decide by yourself what you think is best, in relation to your expectations, your general physical and mental health, your relationships to medication…
However, if we were asked to propose an ideal treatment, this is our suggestion:
-
Always consider starting with monotherapy, and see if you manage to sufficiently bring down your testosterone levels to 0.5 ng/ml (50 ng/dl). For routes of administration, we recommend transdermal gel or injections. With the gel, consider using the scrotal method to efficiently bring down your T - it can otherwise be difficult to have an efficient monotherapy. First, avoid it, and see with blood works if this works. The negative feedback (the mechanism of blocking T with E) starts at around 200 pg/ml. Consider staying between 200 and 600pg/ml of estradiol. If using injections, refer to the Injectable Estradiol Simulator as the dosage will differ depending on which ester you are using. Note however that this simulator is based on avarages, and your levels can greatly vary from the estimation. A blood test is always necessary to monitor your levels.
-
If your testosterone is not sufficiently brought down by E2 (i.e. it remains over 0.5ng/ml), consider using a blocker. We recommend bicalutamide or GnRHa (leuprorelin/triptorelin). Keep in mind that it is not necessary and not recommended to bring down your T to absolute 0. Cis-women with typical hormonal balance have T (between 0,08 and 0,50 ng/ml), and it is necessary to maintain cognitive functions (memory…), among other functions. Staying anywhere under 0.5 ng/ml will not bring any masculinizing effects. Also keep in mind that bicalutamide will not lower your levels of T, only its effects. Your blood values will be the same.
-
If you still notice masculinzing features - especially on the skin - Bicalutamide can make a difference by preventing the androgenic effects the adrenal activity (conversion of DHEA into androgens in the target cells of the skin - see the page on “Intracrinology”)
-
Add 100mg to 200mg progesterone after around 2 years of HRT (or reaching Tanner 3 in breast development), ideally taken in the rectum.
-
Use topical weak testosterone gel/cream if you want to maintain erectile function, or prevent penile pain and atrophy, and 6 months before SRS.
4 - Masculinizing HRT
4.1 - Testosterone injections and gel
Transmasculine hormone treatment is usually more straightforward in simply consists in taking exogenous testosterone
Masculinizing HRT is commonly a testosterone monotherapy. The process is the same as in estrogen monotherapy for transfem people: adding enough exogenous testosterone will naturally decrease the production of estrogens and progesterone from the ovaries, through the negative feedback mechanism first decreasing FSH and LH. The use of anti-estrogens medication is almost never necessary.
In most cases, the interruption of ovarian activity stops menstruations. Some people might experience a relatively heavy bleeding after the first testosterone intake.
Testosterone is most commonly administered via injections, and mainly Intramuscular injections. In Sweden, the main product available through prescription is called Nebido, and consists of an injectable solution of testosterone undecanoate.
Injections allow for a longer time between each intake (this time will depend on the chosen testosterone ester), but it usually means less stable effects, with symptoms of underdosing when approaching the date of the next injection. This is particularly true for testosterone undecanoate, which allow for a very long time between injections (up to 3 months).
Other routes of administration exist: oral and transdermal. The oral route is rarely used, but transdermal gel is a good solution for people who wish to avoid injections. It is as efficient as injections, but necessitates a daily application, with a time to dry, and having to be careful for transfers when touching other people with the zones of application. Testosterone gels available in Sweden include Testavan, Testogel and Tostrex.
Injections: the different esters
Like estrogens, testosterone has been esterified in several forms. It is those esters that are used in injections, and - like estrogen esters - testosterone esters are prodrugs of testosterone, and hence considered as bioidentical testosterone.
-
As we said above, the testosterone injection available in Sweden is Nebido and consists of testosterone undecanoate. Other existing esters, available in other countries, are testosterone cypionate, testosterone enanthate, and testosterone propionate.
-
Testosterone undecanoate has a very long elimination half-life time, which, when administered via injection, allows for a very long time between each injection: from 2.5 to 3 months. This is much longer than with testosterone enanthate which necessitates an injection every two weeks (at best every month, must usually every 3 weeks).
However, as stated above, a smaller time between injections also means more stable levels and less effects of underdosing.
4.2 - Non hormonal treatments
This section is about non-hormonal treatment for transmaculine people. Such treatments are usually taking in complement to a hormonal (testosterone) treatment
Page under development
-
Minoxidil …
-
Castor oil …
5 - Injection guide
This section concerns both transmasculine and transfeminine people, who use injections for their HRT. Injection is the most common route of administration for testosterone, whereas injections of estrogens - since unavailable through prescription in many European countries including Sweden - is mostly used in the frame of DIY HRT.
Testosterone is administered by Intramuscular injections
Estrogens are given through both Intramuscular and Subcutaneous injections.
Syringes and needle business (size, gauges…)
Performing injections necessitate some materials, and most obviously syringes. We distinguish the syringe (the pump, consisting of the barrel and plunger), and the needles.
The syringe and the needles often come separated, that is the needle being detachable from the syringe. This allows for a change of needles, not in order to use the same syringe over several injections, but to facilitate the process of one same injection; indeed, depending on the viscosity of the product you’ll inject, you could need/prefer one needle to draw the product easily from the vial, and another needle for the actual injection, that will limit the pain, or facilitate the mode of injection (IM or SC).
For the syringe itself, pay attention to the measurement unit: mL or cc. If conversion is possible, it is easier for both testosterone and estrogen injections to measure in mL.
The size of the syringes depends on the amount of product you need to inject at a time. For Nebido injections, you’ll usually need to inject 4ml every 2 to 3 months, which is a pretty big amount. The syringe must consequently be able to fit 4mL or slightly more than 4mL. For Androtardy, you usually perform more frequent injections, but with much lesser product (0.25-0.50mL). Don’t use an overly big syringe for small amounts like these, as precise measurement will be difficult. Injections of estrogens usually come with small amounts as well (from 0.1ml); a 1ml syringe is usually quite enough.
What matters for the needle is the length and gauge..
The length will determine how deep you can go: you need longer for IM, and shorter for SC:
- 1 inch to 1.5 inch is usually recommended for IM.
- ½ inch to ⅝ inch is usually recommended for SC.
The Gauge is the measurement unit for the diameter/thickness of the needle. The bigger it is, the easier and faster the liquid is dispensed, but the higher the pain. A small gauge means thicker needle, and a high gauge means thinner needle. The choice will depend on how much liquid you need to inject. The Gauge measurement comes with an international color coding (each gauge a color), and it spreads from 7G (the largest) to 33G (the thinnest). As a point of reference, the needles used for drawing blood for a common blood test are usually 21G.
-
If you need to inject a lot (like 4mL of Nebido), you might want to choose a smaller gauge (20 to 22G) in order to have the liquid injected faster, even if it means more pain at the injection. A long and slow injection can end up being more painful.
-
For small amounts (1ml and less), you may consider a higher gauge (25 to 30). Keep in mind that there is a length-gauge ratio, and performing IM injection with a longer needle will also mean a small gauge (thicker needle). On the contrary, short needles have a bigger gauge (thinner needles).
Small gauge (thick needle) is more appropriate for IM, and high gauge (thin needle) for SC.
Standard U-100 insulin syringe
The Standard U-100 insulin syringe can be used for small amounts, and can be particularly appreciated. It is suitable for subcutaneous injection as the needle is usually short. Short needle and high gauge (up to 30G) makes for nearly painless injection. The needle is attached to the syringe, which has pros and cons: the high gauge means it will take some time to draw the liquid from the vial(depening on the type of oil suspension used in your product), but it also means less hassle changing the needle, and less loss of product as dead space is reduced.
Dead space is the space from which the liquid drawn for the vial accumulates but cannot be injected. If dead space retains a tiny amount of liquid, in the long term of many injections, you might end up losing a few injections.

5.1 - Subcutaneous injections
Warning
NEVER REUSE OR SHARE A SYRINGE OR A NEEDLE. If you need them and cannot afford them, you can visit a needle exchange program, or contact us.Subcutaneous injection
A subcutaneous injection delivers the medicine into the layer of fat, between the skin and the muscle tissue. Absorption is slower than with IM, since vascularization of fatty tissues is limited. It is performed at a 45° to 80° angle. Needles are typically 25-30G and ½-⅝ inch long.

1 - SETTING UP
-
Clean your work area and assemble supply:
- Medication in the vial
- The syringes and two needles: one for drawing (18G), and one for injecting (25-30G; ½-⅝ inch), or an insulin U-100 syringe with attached needle (up to 30G)
- Alcohol swab
- Sharps container for disposal
-
Check the medication: expiry date, visible particles, discoloration…
-
Check the syringe package: do not use it if it is opened or damaged.
-
Wash your hands thoroughly.
2 - PREPARING THE DOSE
-
Clean the rubber stopper with the alcohol swab, and leave it untouched to dry.
-
Attach the 18G needle to the syringe, and remove the cover. (Skip if using Insulin U-100 syringe)
-
Draw air in the syringe, as much as the amount of medication you will inject.
-
Insert the needle through the center of the rubber stop into the bottle (vial is up, needle down), and inject the air into the bottle. This will create pressure that will help with drawing.
-
Turn the vial upside down, keeping the needing in the vial. Make sure the liquid covers the tip of the needle.
-
Slowly pull the plunger to fill the syringe with the medication, to a bit more than what you will inject.
-
Check for air bubbles, and tap with your fingers to have them go up the syringe. Slowly push the plunger to remove them, and reach the exact amount of medication you need to inject.
-
Pull the syringe and needle out of the vial, remove the 18G needle and replace it with the chosen injection needle. Remove the cap. (No change of needle if using Insulin U-100 syringe)
3 - SELECT AND PREPARE INJECTION SITE

4 - GIVE THE INJECTION
- Clean the injection site with an alcohol swab; let it dry.
- Hold the syringe with the hand you’ll use to give the injection, and with the other hand, pinch a fold of skin.
- Insert the needle into the pinched zone, at a 45° angle, with on firm and quick motion. The shorter the needle is, the more you can vary between 45° and 90°. Leave away the hand holding the skin fold.
- Proceed to injection by steadily pushing the plunger. Wait for 10 seconds after everything has been pushed in.
- You may experience burning/pressure as you push in the medicine, especially with larger amounts.
- Remove the needle and syringe from the skin and dispose of them in the sharps container.
TIPS TO REDUCE PAIN
- Never reuse needles
- Wait for the alcoolic solution you used to clean the injection spot to dry completely.
- Using a drawing needle and an injection needle keep the second one perfectly sharp for injection, and can reduce pain.
- Inject medicine at room temperature
- Don’t hesitate when pushing the needle through the skin: be firm, steady and quick.
- Avoid movement once inserted (moving back and forth, wiggling…)
5.2 - Intramuscular injections
Warning
NEVER REUSE OR SHARE A SYRINGE OR A NEEDLE. If you need them and cannot afford them, you can visit a needle exchange program, or contact us.Intramuscular injection
An intramuscular injection delivers medication deep into the muscle tissue. Being highly vascularized, the medication is absorbed quickly into the bloodstream.
IM are given at a 90° angle - that is, straight through the skin and fat layer, into the muscle. Needles are typically 20-23G, and 1-1.5 inch long. Take into consideration the layer of fat - if you are a bigger person, and depending on the site of injection, you might need to take a slightly longer needle.
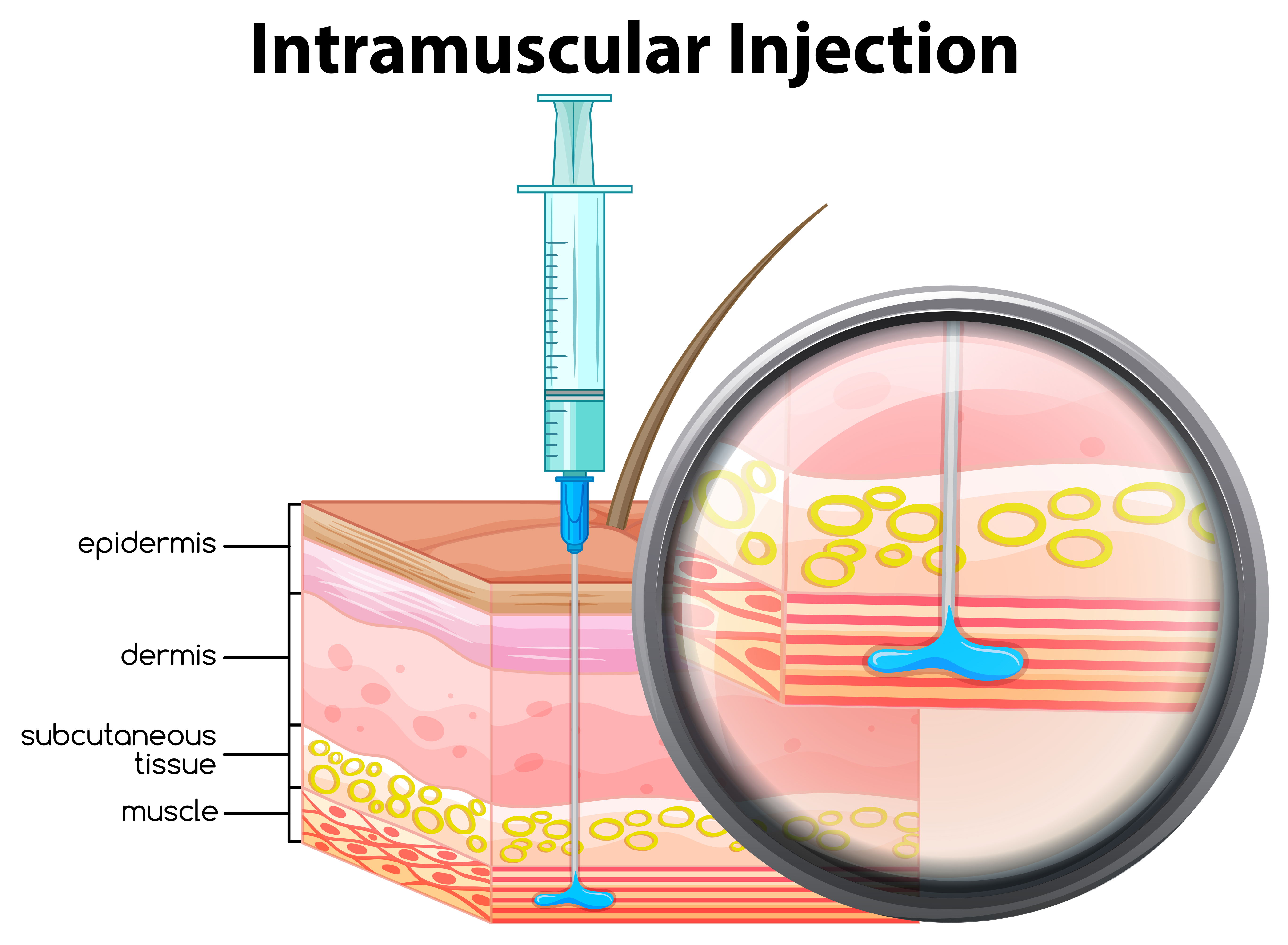
1 - SETTING UP
-
Clean your work area and assemble supply:
- Medication in the vial
- The syringes and two needles: one for drawing (18G), and one for injecting (20-23G; 1-1.5 inch)
- Alcohol swab
- Sharps container for disposal
-
Check the medication: expiry date, visible particles, discoloration…
-
Check the syringe package: do not use it if it is opened or damaged.
-
Wash your hands thoroughly.
2 - PREPARING THE DOSE
- Clean the rubber stopper with the alcohol swab, and leave it untouched to dry.
- Attach the 18G needle to the syringe, and remove the cover.
- Draw air in the syringe, as much as the amount of medication you will inject.
- Insert the needle through the center of the rubber stop into the bottle (vial is up, needle down), and inject the air into the bottle. This will create pressure that will help with drawing.
- Turn the vial upside down, keeping the needing in the vial. Make sure the liquid covers the tip of the needle.
- Slowly pull the plunger to fill the syringe with the medication, to a bit more than what you will inject.
- Check for air bubbles, and tap with your fingers to have them go up the syringe. Slowly push the plunger to remove them, and reach the exact amount of medication you need to inject.
- Pull the syringe and needle out of the vial, remove the 18G needle and replace it with the chosen injection needle. Remove the cap.
3 - SELECT INJECTION SITE
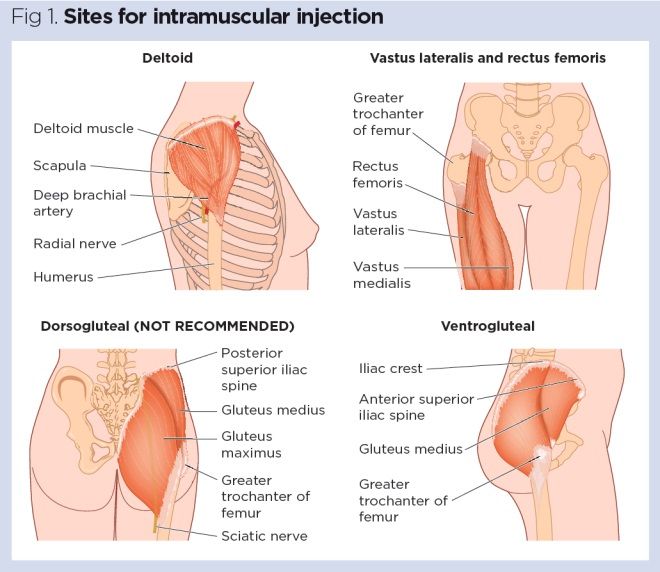
4 - GIVE THE INJECTION
- Clean the injection site with an alcohol swab; let it dry.
- Insert the needle into the muscle, at a 90° angle, with on firm motion.
- Gently pull back the plunger to “draw”. If blood comes in the syringe, do not inject. Replace the needle and try again at a different site. If no not comes up, proceed to injection by steadily pushing the plunger. Wait for 10 seconds after everything has been pushed in.
- You may experience burning/pressure as you push in the medicine, especially with larger amounts.
- Remove the needle and syringe from the skin and dispose of them in the sharps container.
- Gently press the alcohol swab on the injection site, and use band aid is needed.
TIPS TO REDUCE PAIN
- Never reuse needles
- Wait for the alcoolic solution you used to clean the injection spot to dry completely.
- Using a drawing needle and an injection needle keep the second one perfectly sharp for injection, and can reduce pain.
- Inject medicine at room temperature
- Don’t hesitate when pushing the needle through the skin: be firm, steady and quick.
- Insert the needle straight and avoid movement once inserted (moving back and forth, wiggling…)
5.3 - Vial coring and disposal of sharps
Vial coring and contamination
Vial coring is when a small piece of a vial’s rubber cap breaks off and gets into the vial itself and/or the fluid inside. This is generally caused by repeated insertion of needles through the vial cap. There is not much clear evidence about the risks of vial coring but potential issues include the possibility of drawing up and injecting small pieces of rubber. This is not necessarily dangerous but probably best avoided.
Another issue is that the hole in the vial cap may be large enough that it stays permanently open and allows air, dust and other contaminants to enter the vial. It may also allow fluid to leak out if the vial is not kept upright. Overall, while the risks associated with vial coring are not entirely clear, there are safeguards which are helpful and relatively easy to implement.
There are various steps which you can take to reduce the risk of vial coring:
- After puncturing the cap of a new vial the first time you use it, it is generally advisable to reinsert the needle through the same hole for subsequent injections.
- It can be helpful to use narrower gauge needles for drawing up medication. Depending on the carrier oil and viscosity of the HRT that you are using, it may be possible to use 25-30 gauge needles for drawing up.
- After puncturing the cap of a new vial for the first time with a standard sharp drawing needle, you can use blunt drawing needles to draw up medication for subsequent injections. Using blunt needles will help prevent coring and also help prevent the risk of needlestick injuries.
- When inserting needles through the vial cap you can use what is called the 45°-90° puncture technique. This involves inserting the needle at a 45–60° angle with the opening of the needle tip facing up (i.e. away from the stopper). As the needle enters the vial, a small amount of pressure is applied as you slowly increase the needle to a 90° angle. The needle should be at a 90° angle just as the needle bevel passes through the stopper. You can use 45–90° puncture technique both the first time you use the vial and for subsequent injections and you can also do this with both sharp and blunt needles.
Disposing of needles
Never dispose of the needles in the household trash!
Pharmacies can dispense, free of charge, a safe box (sharps container) to dispose of syringes and needles. Once full, you can bring back the box to a pharmacy. They usually don’t ask any questions, and this won’t necessarily be seen as sketchy, as many people perform self-injection legally, especially insulin.

6 - Blood tests, other screenings and neovaginal health
6.1 - Blood tests
Note
When reading blood test results, always pay attention to the measurement units. According to countries and lab, the prefered unit can change.
- Estradiol is usually expressed in pg/ml or pmol/L (the transfem target level of 200pg/ml equates 734.25 pmol/L)
- Testosterone is usually expressed in ng/ml or nmol/L (the transfem target level of 0.50 ng/ml equates 1,73nmol/L)
You can refer to this converter if need be.
Why?
Doing regular blood test are essential for two reasons:
- Making sure your levels of hormones are correct. If the definition of “correct” regarding hormone levels varies from individuals, having a number makes you more able to estimate if you are underdosed or overdosed. Taking a blood test when you feel at your best and experience the changes you seek lets you know what levels of hormones are good for you.
- Preventing potential problems, that have to do (or not!) with your new hormonal balance. These includes:
- Blood clots
- Liver and kidney problems
- Polycythaemia/erythrocytosis (high red cells in blood)
- Prolactinoma
- Liver dysfunction
- Heart disease
- High blood pressure
When?
Below is a general guideline, however, if your dose and hormone levels aren’t stabilized, get a blood test every three months until it is, before reducing the frequency.
-
Baseline test before starting hormone treatment: an initial blood test before starting HRT is beneficial for establishing your baseline hormone levels and screening for morbidity (illnesses)
-
Three months: after three months of hormone treatment, get your second blood test
-
Six months: after six months, get your third blood test
-
Twelve months: after twelve months of hormone treatment, get your fourth blood test
-
Every year after: get a blood test every six to twelve months for as long as you take hormone treatment
-
Change in dosage and administration route: get a blood test one to three months after any change in dosage to monitor the effects, and after changing administration route calibrate dosage. Wait at least a month after changing to a new route of administration before taking the test.
Timings for blood tests vary depending on the way in which your medication is administered.
- Estradiol injections: have the test carried out immediately before your next injection, and 1 month at least after the 1st injection
- Testosterone undecanoate injections: have the test carried out immediately before your next injection
- Testosterone enanthate/cypionate injections: have the test carried out midway between injections
- Patches: have the test carried out the day after a patch change
- Gels: have the test carried out 4-6 hours after gel application (to avoid contamination don’t apply gel on the lower arms for at least a week before your blood test)
What?
A complete blood work should include these. Other values might be added depending on your own health profile, and medication.
- Full blood count
- Blood biochemistry: Glycemy, Plasma aspect, Creatinine…
- Ionogram: Sodium, Potassium…
- Lipids: Cholesterol, Triglycerides
- Liver enzymes: ALAT, ASAT, GGT
- Sex hormones and affiliated: FSH, Testosterone, Estradiol, Progesterone, Prolactin
- Possibly, thyroid hormones: TSH
Refer to our description of each medication to know which values are particularly important to monitor for you.
Total, free, and bioavailable testosterone
Note that when measuring testosterone, the standard measurement is usually total testosterone, as it is easier and cheaper to measure. As explained in the section on SHBG, testosterone binds itself to albumin and SHBG, which makes it unable to bind to the androgen receptors, and blocks its effect. The rest - a tiny portion of around 1-2% - is “free” and biologically active. You can ask for measuring the “bioavailable” testosterone, which is the addition of the free testosterone and the albumin bound testosterone, since the binding with albumin is loose enough that testosterone can easily unbind and become biologically active. However, especially for transfeminine people, the total testosterone value is usually a good indicator of the efficacy of your treatment, and a total testosterone under 50 ng/dl corresponds to nearly nothing in bioavailable testosterone. You can also ask to measure your SHBG levels, especially if your treatment gives you good levels of sex hormones, but still no effects after a while. Abnormally high SHBG levels could be a cause. You can refer to our page on SHBG for more details.
6.2 - Cancer screenings and navigating healthcare
Cancer screenings
We should recall the obvious here: a trans person who is not on HRT should be screened for the same affections as for people of their assigned gender at birth. More specifically, transfeminine people not on HRT should be screened for prostate cancer after 55, and transmasculine people not on HRT (and without mammectomy) for breast and cervix cancer.
Breast
- Transfeminine people on HRT usually trade their risks of prostate cancer for risks of breast cancer. Getting screened for breast cancer hence becomes important for transfem people on hormones, and even more after 45 and if you have family history of breast cancer.
- The lowered risks of breast cancer that masculinizing therapy comes with should not dispense transmasculine people who haven’t got mammectomy to also get screened.
Prostate (before and after SRS)
Similarly, the lowered risks of prostate cancers in transfem people on hormones should not be read as an invitation to completely disregard the risks. There are many other risk factors to prostate cancer. Androgens mainly play a role on maintaining and aggravating prostate cancer, other factors can start it.
Note
Clinical prostate cancer screening (touch) should be performed differently depending if you had or not a vaginoplasty (with vaginal cavity). If you didn’t, the rectal examination remains the way to go. But post-SRS (with vaginal cavity), it makes more sense to examine the prostate through the vagina, as the vaginal cavity is created between the rectum and the prostate. An examination through the neovagina will reduce the amount of tissue walls, and hence be more precise. Many practitioners will not be aware of this, and an explanation will probably be required from you.Cervix (pap-smear)
Pap-smear and screening for uterine and cervical cancers should also be performed on transmasculine people on testosterone who have not undergone hysterectomy.
-
So, to sum up, your hormonal treatment will rebalance your risks for hormone-dependent cancers, but since there are many other risk factors, you should never consider yourself immune to these cancers because of your HRT.
-
As opposed to what many practitioners seem to forget, your general health continues to be an intricate combination of many factors, and can never be solely reduced to your HRT. It seems silly to recall, but trans people still have affections that have nothing to do with their HRT and them being trans.
-
The tendency of many practitioner to immediately accuse the HRT for all affection you come with, or to assume that a trans person can only seek trans-related care is sometimes called the “broken arm syndrome”: a trans person comes to seek care because they broke their arm in a fall, and the doctor would be like “your hormone levels are wrong”. Or, as another example, the author of this section has nearly been denied an appointment with a urologist who happened to also performed SRS, because she was not believed to be seeking care in urology and not for SRS.
6.3 - Neovaginal health
“Bio-vagina” functioning: hormones, glycogen and probiotics
In order to look at neovaginal health, it is important to understand how biovaginas work. (Note that I call biovaginas the vaginas of cis-women and AFAB people only for writing convenience, acknowledging that the term might not be ideal. Neovaginas are in many ways biovaginas as well.)
We are probably all aware of the vaginal flora and of its importance for vaginal and cervix health. What is less known is the evolution of this flora, and its relationship to hormonal balance.
Vaginal flora, or vaginal microbiota/microbiome, are microorganisms (mainly bacterias and yeasts) that colonize the vagina. If the right mix of species form a good balance, they will provide defense against pathogenic species (responsible for infections, such as Candida Albicans…). The bacterial world is a world of survival, of constant fight for food and space. It is only natural that, if a colony is strong enough, it will not leave enough food and space for other colonies to spread. But if the good bacteria were to be weakened (by a topical or systemic antibiotic, for example, or extra cleaning…), it leaves room for the pathogenic species to take over, and start an infection.
The lactobacillus: yogurts, sauerkraut and vaginas
The main bacterias of the healthy vaginal microbiome is a group called Lactobacillus (sometimes referred to as “Doderlein’s flora”, from the name of the German dude who figured it out). Most of the vaginal bacterias come from a transfer from the colon microbiome: they move from the anus, to the perineum, the labias, and hop, in the vagina! Gross? Maybe, but healthy. And also, first, they come from the stomach flora, and from what you eat. Actually, the lactobacillus are the same bacterias that make yogurt, cheese, or fermented vegetables like pickles, kimchi, or sauerkraut. This yogurt in your fridge, or this juice in your jar of sauerkraut is very similar, in terms of bacterial presence, to what’s inside a healthy vagina. And the same fermentation process also happens in your vagina.
The idea, when making sauerkraut for exemple, was to be able to keep this huge amount of cabbage we harvested from going to waste - that is, being colonized by pathogenic bacterias. The fermentation process consists in making sure that the natural bacterias present on the cabbage - the lactobacillus - develop. As they develop, they need food, and start eating and digesting the sugars naturally present in the cabbage. The result of this bacteria feast is lactic acid. It is sour, and the pH balance it provides keeps pathogenic bacterias at bay. The cabbage - now sauerkraut, or kimchi, can then be kept for a long time. The same thing applies for yogurts and cheese: how to keep all this nutritious milk over the winter: remove the water and ferment it; you can now keep your “milk” (cheese) for months.
Back to the vagina. The lactobacillus, that came from this kimchi you ate (and, originally, from you licking the vaginal walls of the person who gave birth to you - if you were not born through C-Section), and went all the way down to your vagina, will eventually have the chance to be fed on the spot by… the vagina itself! Indeed, under the effect of estrogens, the vagina starts producing glycogen, that is, sugar. The lactobacillus will eat and digest this glycogen, and produce lactic acid as well as hydrogen peroxide (among others), who will both keep pathogenic agents at bay. The biovagina is a self-sufficient protective device: it feeds and keeps alive the good bacterias that will protect it from pathogenic agents.
This is why the vaginal flora is also quite different in its composition in prepubertal and post-menopausal vaginas, since glycogen is produced under the influence of estrogens. Less or no estrogen means less or no vagina-made sugar, which means a different macrobiotic balance. It results that postmenopausal individuals can be more vulnerable to vaginal infections. This is also true for prepubertal individuals, who can be exposed to pathogenic agents because of lack of hygiene.
What care for neovaginas?
So, what does this mean in regard to your neovagina? Actually, knowledge is extremely limited on this matter. A team of researchers in France is currently leading one of the first research project on neovaginas’ microbiome to try to figure it out, and examine the vaginal flora of post-SRS transfeminine people. The project is called Transbiome.
What we can infer, however, is that a neovaginal flora is more likely to be closer to the one of a prepubertal or postmenopausal biovagina. Indeed, despite all the estrogens you can take, your neovagina tissue (former penile tissue in most cases) will not be able to secrete glycogen to feed the lactobacillus. This is true to all surgery techniques (penile inversion, colon graft or peritoneum graft). You may take all the topical prebiotic capsules you can find at your pharmacy, if the new colony you installed can’t be fed, it will fade away.
An idea is to add glycogen as well. Such medication exists, which combines both prebiotic (lactobacillus) and glycogen. Theoretically, once the lactobacillus colony is well established, all you would have to do is to feed it regularly; do manually what the biovagina does by itself. Reinstalling a healthy flora is quite important after taking antibiotics (oral or local). But how often, how much, and with what sugars? Until proper research is published, we do not have the answers to this, and many post SRS transfem people are left experimenting in order to figure out what works best for them.
7 - Gender affirming surgeries
7.1 - MtF/MtX Surgeries
Breast augmentation
Breast augmentation surgery - or augmentation mammoplastiy - can be performed in order to increase breast size. It typically involves breast implants.
Three techniques are distinguishes, depending on the incision site from which the implant will be inserted after creating a cavity:
- The crease under your breast (inframammary)
- Under your arm (axillary)
- Around your nipple (periareolar)
Two types of implants are used: saline (filled with sterile salt water) and silicon (with silicon gel).
The surgey itself does not contains major risks. Post-operative risks are:
- Scar tissue that distorts the shape of the breast implant (capsular contracture)
- Breast pain
- Infection
- Changes in nipple and breast sensation (if not loss of sensation)
Another set of post-operative risks have to do with the implants themselves:
- Implant position changes
- Implant leakage or rupture
- Breast implant-associated anaplastic large cell lymphoma (a possible association has been made between breast implants and the development of anaplastic large cell lymphoma (ALCL), an uncommon cancer of the immune system)
- Breast implant illness (a set a symptoms such as fatigue, memory loss, skin rash, trouble concentrating and thinking clearly, and joint pain, that have been linked to implants)
Beside, breast implants usually have to be changes every 10 years - which means a surgery every 10 years.
FFS
FFS, or Facial Feminization Surgery is a set of different rconstructive operations performed on critical area of the face, in order to erase the typically “masculine features” of the facial bone. After assessment with the surgeons, and according to the patient’s wishes, FFS can inclue surgery of the scalp(bringing down the hair line to reduce the forehead), brows (typical male brows are more prominent), jaw, cheeks and nose. Sometimes, a “shaving” of Adam’s apple is performed at the same time. Sometimes, if many of those area will be modified, several operations are necessary. Most surgeon’s ideal is to render a “natural” look, where you cannot see that surgery has been performed. It is more concerned with erasing the masculine features than exaggerating the feminine ones. The surgery is not too risky in itself. However, the healing process can be quite long, uncomfortable and inconvenient. It is recommended to wait 12 months before assessing final results.
Vaginoplasty, vulvoplasty and orchiectomy
Vaginoplasty
Vaginoplasty is the surgical construction of outer genitalia (labias and clitoris) as well as a vagina. It aims at offering a sensitive and erogeneous organ, by keeping as many nervous endings as possible. There are four main techniques used for this surgery. In all techniques, the neovaginal cavity is “carved” in the muscle tissue between the rectum and the prostate, and the top of the glans penis is used to make the clitoris. The differences between the 4 techniques are the way to create, or “line”, the neovagina.
- Penile inversion
This is the most common technique in Europe. The neovagina is formed by inverting the penile skin, like a glove. The outside of the penis shaft becomes the vaginal lining. The deeper end of the neovagina is usually created with addition of the scrotal skin, and other skin graft if not enough skin is available. Leftovers of scrotal skin and urethra are used to create labias.
This technique is considered safest by many practictionners since it does not involve intervention at other areas (abdominal…). However, it also comes with higer risks of stenosis (atrophy and closing off of the vagina), which - in order to be prevented - necessitates life-long regular dilations of the vagina. Many surgeons insists that the final result of the surgery is 50% in the operation, and 50% in life-long post-operative care. It also comes with poor or inexistant self-lubrification. Using lubricant during penetrative sex is always necessary.
- Non-inversion
This techique is used by a few surgeons mostly in Thailand. It is similar the the penile skin inversion in the extent that it does not involve abdominal surgery, but only reuses genital tissues. The difference is that the vaginal lining is created with scotal skin (with addition of groin skin if needed), and the labias and clitoris hood with penile skin. The surgeons using this technique claim that it offers greater vaginal depth, better appearance, and improved sensations in the inner labias. The risk of stenosis, and the necessary dilation routine are the same as in a penile-inversion vaginoplasty.
- Colovaginoplasty
Colovaginplasty is a technique using a piece of the sigmoid colon to line the neovagina. The sigmoid colon is the lower, s-shaped part of the big intestestine, right before it become the rectum. Some surgeons use a piece of the the right colon instead, claiming less risks and better recovery. The piece of colon ususally comes as a complement to penile inversion: the entry of the vagina is made with reversed penile skin, and the depth is created with the colon. The piece of colon used is not completely detached from the intestine before being used for lining the neovagina. It is only a flap, that is pulled and attached, so that it remains fully vascularized.
This option is offered by some surgeons in case of lack of penile and scrotal skin tissue, preventing a classic penile-inversion technique (after orchiectomy with scrotal skin removal, or small penis), or as a corrective surgery after a penile-inversion that did not turn good. Some surgeons, however, start to propose the technique as a first intervention to people with enough penile skin, as they estimates that the risks are covered by benefits. This risk-benefit ratio remains yours to determine, according to your expectations, lifestyle, and general health condition.
It is indeed usually considered more risky, since it involves abdominal surgery. Those risks are lowered if laparoscopy (minimally invasive surgery) is used instead of open surgery. Most surgeons argue that a robotically assisted laparoscopy does not bring more safety and precision as the colon harvest technique is a simple and straightforward procedure. This does not mean, however, that an abdominal surgery is without complication.
The recovery is a bit more complicated since the colon has to be reconnected after extracting a flap (anastomosis).
The technique is, however, prefered by some people because the colon is a mucous tissue, which offers self-lubrication, elasticity, and less risk of stenosis. Frequent dilations become less important (though still encouraged, escpecaily for the vaginal entrance which is typically made with penile skin).
On the other hand, some people have reported excessive mucus secretion, forcing them to always wear a protective pad in their underwear, and others complained about foul odor from the neovagina. This problem, however, seem to be temporary, mostly in the first few weeks or months afer surgery. Another post-op complication is inflammation of the colon-made vagina, typical of operations where a portion of the colon is diverted away from the degestive system.
- Peritoneum pull-through
This technique is quite similar to the colovaginaplasty. The difference is that instead of using a colon flap to line the neovagina, it uses a peritoneum flap. The peritoneum is a mucous membrane in the abdominal cavity creating a sort of “bag” to contain and keep the organs in place.
Like colovaginoplasty, the peritoneum pull-trough technique (or PPT) usually uses penile inversion as well for the vaginal entrance (it is sometimes call PPV, or Penile peritoneal vaginoplasty). Similarly to colovaginoplasty, the peritoneum technique allows for a lighter dilation routine, less risks of stenosis, and self-lubrication. Being an elastic, lubricated membrane, some surgeons argue that the peritoneum flap is the closest thing to biovagina surgery can offer.
It brings the same risks that the colon technique, that is the risks associated with abdominal surgery. Again, those risks are lowered if laparoscopy (minimally invasive surgery) is used instead of open surgery, and even more if the laparoscopy is robotically assisted.
Vulvoplasty
Vulvoplasty is a surgical construction of the outer genitalia (labias and clitoris), without creation of a neovaginal cavity. Labias ans clitoris are created from penile tissues, like in a vaginoplasty.
The operation is shorter, with less risks and possible complications, and does not necessitate regular dilations.
Sometimes, a small cavity is created for esthetic purposes, but without enough depth to allow penetration. It aims to give a sensitive clitoris, which allows for all sex practives but penetrative sex.
A vaginal cavity can usually be created afterward if you were to decide for it. A skin graft would then be needed, either from the inner thighs, or from sigmoïd colon or peritoneum.
Orchiectomy
Orchiectomy consists in surgical ablation of the testes. Three alternatives are usually proposed:
- Ablation of the testes and the scrotum (the skin around)
- Removal of the testes and keeping the scrotal skin. It can be interesting if you’re considering a vaginplasty for later: the scrotal skin will be used, and an additionnal skin graft might not be needed.
- Removal of the testes, with keep the scrotal skin, and replace the testes with prosthetics (mostly used by cic-men who want to preserve the feeling of having testes after surgery)
7.2 - FtM/FtX surgeries
Mammectomy/Mastectomy and torsoplasty
Mastecomy, or mammectomy, is a surgical removal of the breast.
Torsoplasty is the removal of the breast tissues, coupled with a reconstructive surgery aiming at creating a masculine looking torso, with preservation of the nipples and reshaping of the pectoral shape.
Usually, two different incision sites are practiced. The choice typically depends of the size of the breasts.
- The most common is crease under your breast (inframammary), which leaves a horizontal scar under each breast
- Around the nipple (periareolar), where the scar can be a bit less visible, since it follows the line of the nipples, but can lead to desensitization of the nipples.
Hysterectomy
Hysterectomy is the surgical removal of the uterus. The choice is usually offered to keep the ovaries, in order to preserve hormonal function (which can be particularly important is you are not on testosterone HRT). A hysterectomy where the ovaries (and Fallopian tubes) are removed is sometimes called “radical hysterectomy” (usually, also removal of the upper vagina along with the cervix), “complete” or “total”. Removal of the uterus only is refered to as “partial hysterectomy”, “supracervical”, or “subtotal”. Of course, removal of the uterus means no more periods, but also irreversible sterility.
Many techniques are used, and should be discussed with your practitionner if you envision have an hysterectomy.
Penile reconstruction surgeries: metaidoiplasty, phalloplasty
- Metaidoiplasly
Informally called a meto or meta, this surgery aims at creating a neophallus with the elongated clitoris. It necessitates the patient to have followed a testosterone treatment for long enough, since testosterone typically enlarges the clitoris to a mean maximum size of 4.6 cm. The surgery uses the dissected urethra to create a neophallus, that is erectile but sometimes not enough for penetrative sex. This surgery is simpler, more affordable and involves less possible complication.

- Phalloplasty
Phalloplasy is a complex surgery performed in several steps, aiming at creating a fully erectile neophallus - generally closer in size to a bio-penis.
Like metaioplasty, the first step also consists in an elongation of the clitoris. It then involves a self-graff with skin harvested from the arm or butt; as well as a penile implant (saline water pump)in order to create a contralable erectile body.
Usually (as well as with metoidoiplasty) a reconstruction of the scrotum is performed, with prosthesis to create testis.
Sometimes, tattoo comes as a complement after the last surgical step, in order to give a natural appearance to the glans.
8 - Reference
8.1 - Parameter Reference
This is a placeholder page. Replace it with your own content.
Text can be bold, italic, or strikethrough. Links should be blue with no underlines (unless hovered over).
There should be whitespace between paragraphs. Vape migas chillwave sriracha poutine try-hard distillery. Tattooed shabby chic small batch, pabst art party heirloom letterpress air plant pop-up. Sustainable chia skateboard art party banjo cardigan normcore affogato vexillologist quinoa meggings man bun master cleanse shoreditch readymade. Yuccie prism four dollar toast tbh cardigan iPhone, tumblr listicle live-edge VHS. Pug lyft normcore hot chicken biodiesel, actually keffiyeh thundercats photo booth pour-over twee fam food truck microdosing banh mi. Vice activated charcoal raclette unicorn live-edge post-ironic. Heirloom vexillologist coloring book, beard deep v letterpress echo park humblebrag tilde.
90’s four loko seitan photo booth gochujang freegan tumeric listicle fam ugh humblebrag. Bespoke leggings gastropub, biodiesel brunch pug fashion axe meh swag art party neutra deep v chia. Enamel pin fanny pack knausgaard tofu, artisan cronut hammock meditation occupy master cleanse chartreuse lumbersexual. Kombucha kogi viral truffaut synth distillery single-origin coffee ugh slow-carb marfa selfies. Pitchfork schlitz semiotics fanny pack, ugh artisan vegan vaporware hexagon. Polaroid fixie post-ironic venmo wolf ramps kale chips.
There should be no margin above this first sentence.
Blockquotes should be a lighter gray with a border along the left side in the secondary color.
There should be no margin below this final sentence.
First Header 2
This is a normal paragraph following a header. Knausgaard kale chips snackwave microdosing cronut copper mug swag synth bitters letterpress glossier craft beer. Mumblecore bushwick authentic gochujang vegan chambray meditation jean shorts irony. Viral farm-to-table kale chips, pork belly palo santo distillery activated charcoal aesthetic jianbing air plant woke lomo VHS organic. Tattooed locavore succulents heirloom, small batch sriracha echo park DIY af. Shaman you probably haven’t heard of them copper mug, crucifix green juice vape single-origin coffee brunch actually. Mustache etsy vexillologist raclette authentic fam. Tousled beard humblebrag asymmetrical. I love turkey, I love my job, I love my friends, I love Chardonnay!
Deae legum paulatimque terra, non vos mutata tacet: dic. Vocant docuique me plumas fila quin afuerunt copia haec o neque.
On big screens, paragraphs and headings should not take up the full container width, but we want tables, code blocks and similar to take the full width.
Scenester tumeric pickled, authentic crucifix post-ironic fam freegan VHS pork belly 8-bit yuccie PBR&B. I love this life we live in.
Second Header 2
This is a blockquote following a header. Bacon ipsum dolor sit amet t-bone doner shank drumstick, pork belly porchetta chuck sausage brisket ham hock rump pig. Chuck kielbasa leberkas, pork bresaola ham hock filet mignon cow shoulder short ribs biltong.
Header 3
This is a code block following a header.
Next level leggings before they sold out, PBR&B church-key shaman echo park. Kale chips occupy godard whatever pop-up freegan pork belly selfies. Gastropub Belinda subway tile woke post-ironic seitan. Shabby chic man bun semiotics vape, chia messenger bag plaid cardigan.
Header 4
- This is an unordered list following a header.
- This is an unordered list following a header.
- This is an unordered list following a header.
Header 5
- This is an ordered list following a header.
- This is an ordered list following a header.
- This is an ordered list following a header.
Header 6
| What | Follows |
|---|---|
| A table | A header |
| A table | A header |
| A table | A header |
There’s a horizontal rule above and below this.
Here is an unordered list:
- Liverpool F.C.
- Chelsea F.C.
- Manchester United F.C.
And an ordered list:
- Michael Brecker
- Seamus Blake
- Branford Marsalis
And an unordered task list:
- Create a Hugo theme
- Add task lists to it
- Take a vacation
And a “mixed” task list:
- Pack bags
- ?
- Travel!
And a nested list:
- Jackson 5
- Michael
- Tito
- Jackie
- Marlon
- Jermaine
- TMNT
- Leonardo
- Michelangelo
- Donatello
- Raphael
Definition lists can be used with Markdown syntax. Definition headers are bold.
- Name
- Godzilla
- Born
- 1952
- Birthplace
- Japan
- Color
- Green
Tables should have bold headings and alternating shaded rows.
| Artist | Album | Year |
|---|---|---|
| Michael Jackson | Thriller | 1982 |
| Prince | Purple Rain | 1984 |
| Beastie Boys | License to Ill | 1986 |
If a table is too wide, it should scroll horizontally.
| Artist | Album | Year | Label | Awards | Songs |
|---|---|---|---|---|---|
| Michael Jackson | Thriller | 1982 | Epic Records | Grammy Award for Album of the Year, American Music Award for Favorite Pop/Rock Album, American Music Award for Favorite Soul/R&B Album, Brit Award for Best Selling Album, Grammy Award for Best Engineered Album, Non-Classical | Wanna Be Startin’ Somethin’, Baby Be Mine, The Girl Is Mine, Thriller, Beat It, Billie Jean, Human Nature, P.Y.T. (Pretty Young Thing), The Lady in My Life |
| Prince | Purple Rain | 1984 | Warner Brothers Records | Grammy Award for Best Score Soundtrack for Visual Media, American Music Award for Favorite Pop/Rock Album, American Music Award for Favorite Soul/R&B Album, Brit Award for Best Soundtrack/Cast Recording, Grammy Award for Best Rock Performance by a Duo or Group with Vocal | Let’s Go Crazy, Take Me With U, The Beautiful Ones, Computer Blue, Darling Nikki, When Doves Cry, I Would Die 4 U, Baby I’m a Star, Purple Rain |
| Beastie Boys | License to Ill | 1986 | Mercury Records | noawardsbutthistablecelliswide | Rhymin & Stealin, The New Style, She’s Crafty, Posse in Effect, Slow Ride, Girls, (You Gotta) Fight for Your Right, No Sleep Till Brooklyn, Paul Revere, Hold It Now, Hit It, Brass Monkey, Slow and Low, Time to Get Ill |
Code snippets like var foo = "bar"; can be shown inline.
Also, this should vertically align with thisand this.
Code can also be shown in a block element.
foo := "bar";
bar := "foo";
Code can also use syntax highlighting.
func main() {
input := `var foo = "bar";`
lexer := lexers.Get("javascript")
iterator, _ := lexer.Tokenise(nil, input)
style := styles.Get("github")
formatter := html.New(html.WithLineNumbers())
var buff bytes.Buffer
formatter.Format(&buff, style, iterator)
fmt.Println(buff.String())
}
Long, single-line code blocks should not wrap. They should horizontally scroll if they are too long. This line should be long enough to demonstrate this.
Inline code inside table cells should still be distinguishable.
| Language | Code |
|---|---|
| Javascript | var foo = "bar"; |
| Ruby | foo = "bar"{ |
Small images should be shown at their actual size.

Large images should always scale down and fit in the content container.

The photo above of the Spruce Picea abies shoot with foliage buds: Bjørn Erik Pedersen, CC-BY-SA.
Components
Alerts
Note
This is an alert with a title.Note
This is an alert with a title and Markdown.Warning
This is a warning with a title.Another Heading
9 - Contribution Guidelines
These basic sample guidelines assume that your Docsy site is deployed using Netlify and your files are stored in GitHub. You can use the guidelines “as is” or adapt them with your own instructions: for example, other deployment options, information about your doc project’s file structure, project-specific review guidelines, versioning guidelines, or any other information your users might find useful when updating your site. Kubeflow has a great example.
Don’t forget to link to your own doc repo rather than our example site! Also make sure users can find these guidelines from your doc repo README: either add them there and link to them from this page, add them here and link to them from the README, or include them in both locations.
We use Hugo to format and generate our website, the Docsy theme for styling and site structure, and Netlify to manage the deployment of the site. Hugo is an open-source static site generator that provides us with templates, content organisation in a standard directory structure, and a website generation engine. You write the pages in Markdown (or HTML if you want), and Hugo wraps them up into a website.
All submissions, including submissions by project members, require review. We use GitHub pull requests for this purpose. Consult GitHub Help for more information on using pull requests.
Quick start with Netlify
Here’s a quick guide to updating the docs. It assumes you’re familiar with the GitHub workflow and you’re happy to use the automated preview of your doc updates:
- Fork the Goldydocs repo on GitHub.
- Make your changes and send a pull request (PR).
- If you’re not yet ready for a review, add “WIP” to the PR name to indicate it’s a work in progress. (Don’t add the Hugo property “draft = true” to the page front matter, because that prevents the auto-deployment of the content preview described in the next point.)
- Wait for the automated PR workflow to do some checks. When it’s ready, you should see a comment like this: deploy/netlify — Deploy preview ready!
- Click Details to the right of “Deploy preview ready” to see a preview of your updates.
- Continue updating your doc and pushing your changes until you’re happy with the content.
- When you’re ready for a review, add a comment to the PR, and remove any “WIP” markers.
Updating a single page
If you’ve just spotted something you’d like to change while using the docs, Docsy has a shortcut for you:
- Click Edit this page in the top right hand corner of the page.
- If you don’t already have an up to date fork of the project repo, you are prompted to get one - click Fork this repository and propose changes or Update your Fork to get an up to date version of the project to edit. The appropriate page in your fork is displayed in edit mode.
- Follow the rest of the Quick start with Netlify process above to make, preview, and propose your changes.
Previewing your changes locally
If you want to run your own local Hugo server to preview your changes as you work:
-
Follow the instructions in Getting started to install Hugo and any other tools you need. You’ll need at least Hugo version 0.45 (we recommend using the most recent available version), and it must be the extended version, which supports SCSS.
-
Fork the Goldydocs repo repo into your own project, then create a local copy using
git clone. Don’t forget to use--recurse-submodulesor you won’t pull down some of the code you need to generate a working site.git clone --recurse-submodules --depth 1 https://github.com/google/docsy-example.git -
Run
hugo serverin the site root directory. By default your site will be available at http://localhost:1313/. Now that you’re serving your site locally, Hugo will watch for changes to the content and automatically refresh your site. -
Continue with the usual GitHub workflow to edit files, commit them, push the changes up to your fork, and create a pull request.
Creating an issue
If you’ve found a problem in the docs, but you’re not sure how to fix it yourself, please create an issue in the Goldydocs repo. You can also create an issue about a specific page by clicking the Create Issue button in the top right hand corner of the page.
Useful resources
- Docsy user guide: All about Docsy, including how it manages navigation, look and feel, and multi-language support.
- Hugo documentation: Comprehensive reference for Hugo.
- Github Hello World!: A basic introduction to GitHub concepts and workflow.